Presentation: late-20s male, denied any medical history, presented after he got hit multiple times in the head with a two-by-four when he drunkenly stumbled into a stranger’s yard while walking home. He had some abrasions to the head and face, and was obviously intoxicated, but had normal vitals and a nonfocal neurologic exam. He had no visible trauma to the extremities or torso on initial evaluation and had reportedly been ambulatory at the scene. He was cooperative and really wasn’t causing too much trouble for an EXI patient on whatever night it was. So I went with the “liter of fluids, basic labs, scan his head and c-spine, and watch him while he sobers up” approach. It’s one I’ve used many times before and since, and one that in all honesty I still stand by for this patient, at least initially.
Fast forward a handful of hours, his scans are negative, and he’s sobered up nicely. He’s still cooperative, but having a little bit of left side pain. He wasn’t very hungry but had taken a few sips and tolerated them okay. So our fabulous nurse and tech tell me he’s “walky-talky” and probably going to be ready to go soon. I start to get his discharge ready, when they catch my eye and call me over.
What I see when I get over there is not at all what I expect based on my last spin through EXI on my way out of Room 9…
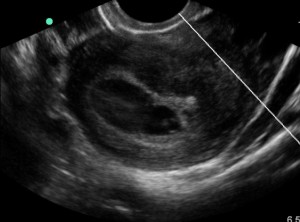
Now, this guy looks sick. Legitimately sick. Not just unsteady or a little too drunk to walk, he is GHOSTLY pale and unable to stand. He’s got a pained grimace on his face and is about to pass out. We got him back into his chair and someone went off to grab an extra bag of fluids and the ultrasound for me, since his heart rate had spiked up to 125. After he was flat in his chair, I threw the ultrasound probe on his abdomen: RUQ was equivocal, but his LUQ had a nice huge stripe of free fluid. He also had some new ecchymosis in his left lateral abdomen/LUQ. Unfortunately I was in a little bit of panic mode and didn’t save his ultrasound images, but it was crystal clear to me what had happened: something had been bleeding for a while and was now causing a big problem. So we rolled his chair into Room 9, plopped him onto a bed, and hit the Level I button when his manual systolic pressure came out at 85. We pumped fluids in him and got blood to the bedside and into his veins right about the same time the wedge and chief showed up. He stabilized enough for the scanner after initial resuscitation, and Trauma stood by in radiology to watch the images come up.
His spleen was pretty much ripped in two. He didn’t appear to have any active extravasation (surprisingly, as far as I recall), and his pressure was improving though his heart rate wouldn’t go below 100 for more than a few seconds at a time. I talked to him, I talked to his mother, and I talked to the Trauma folks. We had enough time to get repeat blood work, discuss the impending surgery, and get him packaged up as stable as he was going to be before they whisked him away to Room 4 (or maybe 6, whichever).
He recovered uneventfully from his splenectomy, and was discharged from the hospital a few days later. He had the best possible outcome given the particulars of his eventful time in the ER. But I kept asking myself a handful of questions over the following days that I still think about from time to time. What if we had walked him earlier, well before his hemorrhage was on the border of Class II and Class III? Could he have gone home and died of hemorrhagic shock from a missed spleen injury? What if I had scanned him earlier and he had only had a tiny contained rupture with no extravasation? Would he have ended up in OR 4 anyway but gone there from the floor or PCU instead of from the ED? How should I have proceeded differently?
After kicking myself for a couple of days, I talked with the attending who had been on with me at the time all of the kerfuffle went down, and felt much better about my decision-making process. I distinctly remember him having no torso trauma or pain on my first assessment. Man scanning this young, otherwise healthy patient was not indicated. It was not contraindicated, but would have seemed superfluous and a misuse of resources based on his initial presentation. As a side note, which was honestly extremely relieving to me, Trauma wasn’t all that critical of my decision-making process and was just glad we caught it before it got any worse.
In doing a little bit of background research, it appears that delayed spleen rupture is a not-entirely-unheard-of entity, but is debated in some surgical literature as a term coined as an alternative way to describe a missed initial diagnosis. Regardless of what it’s called, it does happen. Though, when it does, it’s usually after at least a couple of days (sometimes even a week), not just a few hours. The literature focuses more on whether it’s a legitimate problem than how to manage, as the management is no different from a normal spleen rupture. Operative intervention is the usual course, though some small lacerations/subcapsular hematomas are electively managed with observation first, especially in high-operative-risk patients.
My experience gave me 3 lessons to take away.
First: Young, healthy, adult patients can trick you just like children, with vitals not markedly abnormal until a big problem is present. So you need to reassess them. I know I’m as guilty as the next person of not always reassessing as thoroughly as I’d like, especially on a busy shift, but I’m also much more aware of who will need me to do a little more work before I can bless their departure.
Second: Drunk (or otherwise intoxicated patients) can trick you and hide serious problems. Be aware of this going forward, because it doesn’t mean you need to man scan everyone, it just means you need to keep your mind open to injuries that aren’t initially apparent.
Third: Adjusting the plan and course is entirely okay, and in some ways it’s what EM is built for. It’s why we get gaits on traumas with leg pain. It’s why we walk our drunks and PO challenge our vomiting patients. And it’s something we have to keep in mind because we’ve all seen patients who went from apparently fine to nearly-dead in what seemed like a single instant.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)
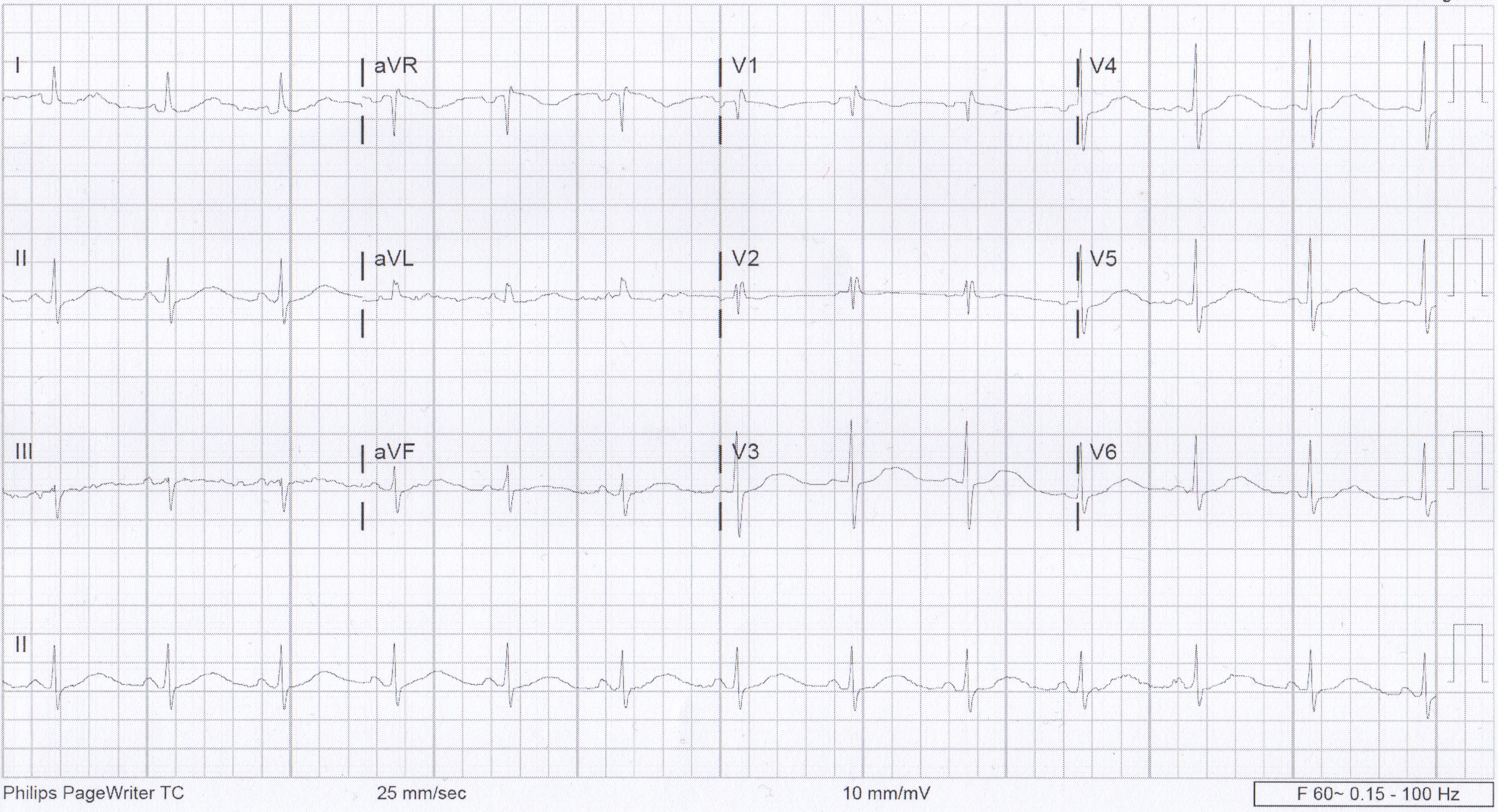
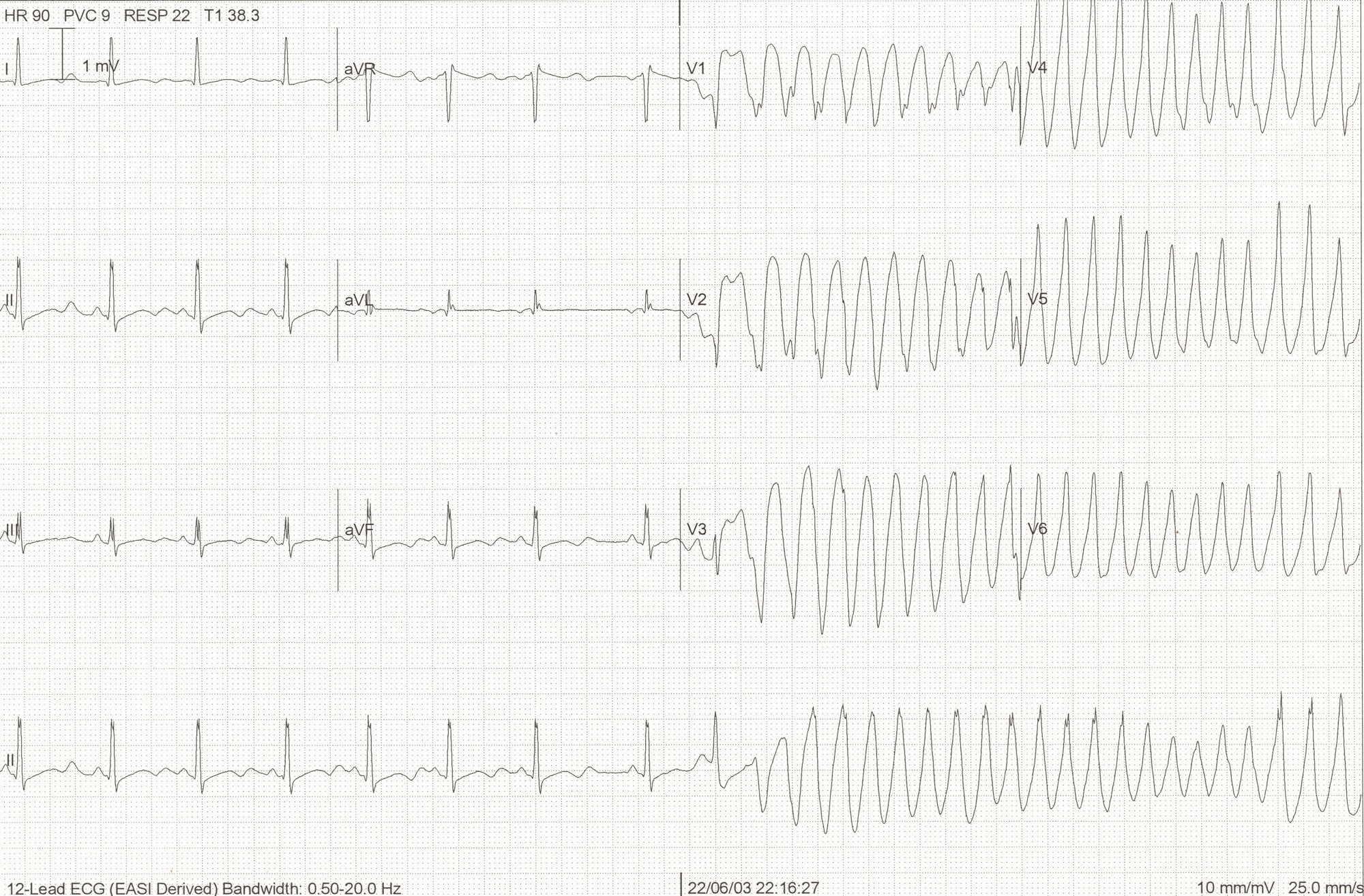
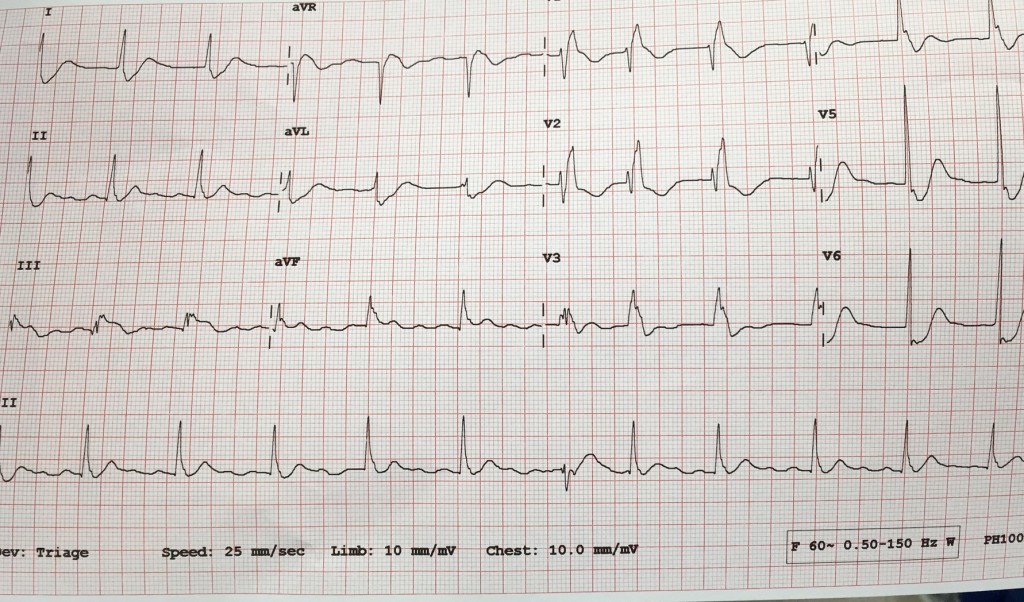
 We usually talk about QTc rather than just the QT. This is because the QT interval varies depending on the HR. Using a correction equation standardizes the interval so it can be interpreted regardless of the HR. The EKG computer does give a calculation of the QTc, because we are obviously not hand calculating this on every patient. You should compare what the computer calculates to your gestalt when you review the EKG. If there are any concerns or discrepancies, you should hand calculate the QTc.
We usually talk about QTc rather than just the QT. This is because the QT interval varies depending on the HR. Using a correction equation standardizes the interval so it can be interpreted regardless of the HR. The EKG computer does give a calculation of the QTc, because we are obviously not hand calculating this on every patient. You should compare what the computer calculates to your gestalt when you review the EKG. If there are any concerns or discrepancies, you should hand calculate the QTc.