…forever seeking the unsuspecting emergency medicine intern.
A previously healthy teenage male presented to the emergency department via emergency medical services with the complaint of weakness, sensory changes, and increasing difficulty of breathing. Family reported the patient went outside to mow the grass approximately 10 hours prior to presentation. After two passes in the yard with a push mower, the patient had sudden onset occipital headache, fatigue, parasthesias described as tingling in both lower extremities, and generalized weakness. Patient reported these symptoms to parents and laid down to rest. After an hour long nap, patient was encouraged to take a shower to see if symptoms improved. During shower, patient became weaker, had one episode of vomiting and was no longer able to stand on legs. The patient’s father reports patient was able to make small movements but unable to ambulate or push against resistance. Emergency medical services were contacted at this point, however, after assessment, the symptoms were deemed related to anxiety and patient was not transported. Over the course of the day, the patient’s weakness progressed to the complete inability to move legs, followed by inability to move arms, with continued paresthesias in all extremities. After patient demonstrated worsening respiratory distress, EMS was called again. Parents denied history of asthma, prior wheeze, fevers, recent illness or trauma, recent travel or drug abuse. Family reports patient went camping one week prior but denies tick exposure.
On exam, the patient had significant respiratory distress with poor air movement and was only able to answer questions with one word responses secondary to respiratory distress. Neurological exam revealed 0/5 strength in all extremities, areflexic biceps and brachioradialis reflexes, areflexic patellar and Achilles reflexes, and downward going Babinski bilaterally. Sensation to light touch was intact but diminished in all extremities. There were no rashes or lesions on skin exam.
Initial differential included but was not limited to:
- Organophosphate toxicity – although patient self-decontaminated earlier in the afternoon and did not have diarrhea, salivation, or lacrimation
- Guillain Barre – although acute time course without report of recent URI or GI syndromes
- Tick paralysis – although no known exposure or lesions identified on skin or scalp
- Transverse Myletitis – although no personal history of recent illness, no family history of multiple sclerosis or other autoimmune disease
- Spinal Cord Infarct – although patient and family deny trauma, recent surgery, or history of coagulation disorder
- Conversion Disorder – although no anxiety or other psychiatric history
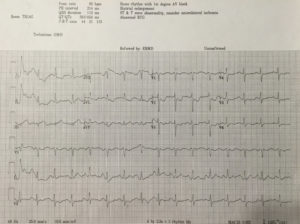
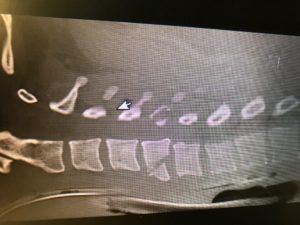
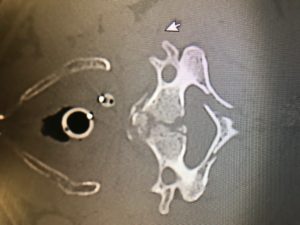
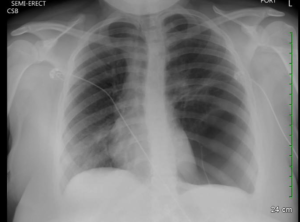
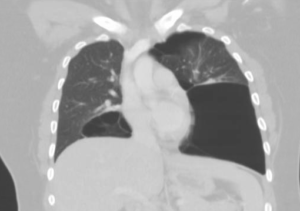
As concern for bronchospasm, the patient was given IM epinephrine and started on a hour long albuterol while history was being obtained. Bedside ultrasound demonstrated grossly normal myocardial contractility without effusion, normal lung sliding, and a collapsible IVC. Chest x-ray was unrevealing. After lack of improvement with initial intervention, second dose of epinephrine and fluid bolus begun. Intial VBG demonstrated hypercapnea and patient was started on BiPAP. Within minutes, patient showed improvement in respiratory status and appeared more comfortable. Initial CMP, CBC, CRP, and ESR were unrevealing. Lumbar puncture was performed after head CT revealed only an arachnoid cyst. CSF studies demonstrated mildly elevated segs, mildly elevated glucose, negative gram stain and normal protein. Foley catheter was placed after patient complained of bladder fullness (confirmed by bladder scan) with inability to void. Neurology and Neurosurgery were consulted from the emergency department, who requested urgent MRI on admission. Patient was admitted to PICU with ED diagnoses of acute flaccid paralysis and acute neuromuscular respiratory failure. After admission, MRI was obtained and demonstrated (drum roll please) ischemia vs. infarct from approximately C2-T5 with predominance in the anterior horns.
The literature review of non-traumatic spinal cord infarction is as rare as the pathology itself in the pediatric population and predominately consists of case studies. Causes typically include but are not limited to hypotension, vascular injury, thrombus, embolus or compression. Considering many of these etiologies are already scarce in the pediatric population, finding cause proves to be a difficult task. Pain in neck, back or legs, weakness, tingling, and numbness are commonly described symptoms in pediatric case studies and were present in the patient that presented to us. Prognosis studies have been performed on primarily adult patients; one such study demonstrated >40% recovery in ambulation amongst the 37 patients that left the hospital wheelchair bound through aggressive physical therapy and rehabilitation programs.[1] Poor prognostic factors include female sex, advanced age, severity of symptoms, and lack of improvement within 24 hours after infarction.[2] It appears as though outcomes are primarily dependent on access to physical therapy and supportive care including psychological treatment. Workup and treatment recommendations if suspicious of atraumatic spinal cord infarct include obtaining an MRI for definitive diagnosis, followed by autoimmune, hypercoagulable, and infectious evaluations. Treatment in the emergency department is mostly supportive and includes addressing any contributory conditions and the management of respiratory concerns.[3]
On follow up, I found that the patient required intubation after exhibiting respiratory decompensation after the MRI was obtained. Initial treatment with high-dose steroids and IVIG were discontinued when infectious and immunologic work-ups were unrevealing. The hospital course was complicated by neurogenic bowel and bladder, neuropathic pain, anxiety, intermittent autonomic instability with hypotension, pneumonia and a urinary tract infection. The patient required tracheostomy and percutaneous gastric tube placement during his hospital stay. The patient continued to exhibit flaccid paralysis of all four extremities and ventilator dependence on discharge to acute rehabilitation.
Per my own investigation, I was relieved to find that Frazier has both success managing these cases and many unique resources that may positively impact this patient’s course (if you are curious here is some video evidence https://www.youtube.com/watch?v=8o_w174rI3s). Needless to say, my differential for motor weakness, particularly in pediatrics, will forever be haunted by this case.
[1] Robertson CE, Brown RD Jr, Wijdicks EF, et al. Recovery after spinal cord infarcts: long-term outcome in 115 patients. Neurology. 2012; 78: 114–121.
[2]Cheshire WP, Santos CC, Massey EW, Howard JF Jr . Spinal cord infarction: etiology and outcome. Neurology. 1996;47(2):321.
[3] Spencer, Sandra P. MD; Brock, Timothy D. MD; Matthews, Rebecca R. MD; Stevens, Wendy K. MD. Three Unique Presentations of Atraumatic Spinal Cord Infarction in the Pediatric Emergency Department Pediatric Emergency Care. 30(5):354-357, May 2014.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)