Emergency Management of Dentition and Midface
- Dentoalveolar trauma can include fractures, avulsions, displacement of teeth
- An avulsed tooth is only viable within one hour, however, even outside of this window it is still worth replacing the tooth. In some cases, they may then get a root canal with dentistry
- Alveolar fractures need timely treatment or risk poor cosmetic outcome and infection
- Most oral abscesses can be drained in the ED with close dental follow-up
- The need to obtain CT is dependent on the full clinical picture. If pt has significant RFs for deep space infection or cancer, it may warrant a face CT
- Trismus sometimes can be confused with guarding due to pain. Can be worthwhile to provide analgesia and reassess
- Buccal and canine space infections can present with significant facial swelling. These should be assessed with CT, drainage should occur from within the oral cavity near the involved tooth, not through the skin of the face
- Radiology reads will frequently indicate Ludwig’s, however, this is often overread. True Ludwig’s is a surgical emergency. Can cause significant airway compromise
- As a general approach to anesthetic for oral abscesses, should first infiltrate around the abscess, then can attempt direct injection
- Inferior alveolar N blocks can be challenging due to surrounding vessels as well as the parotid gland that can be inadvertently damaged
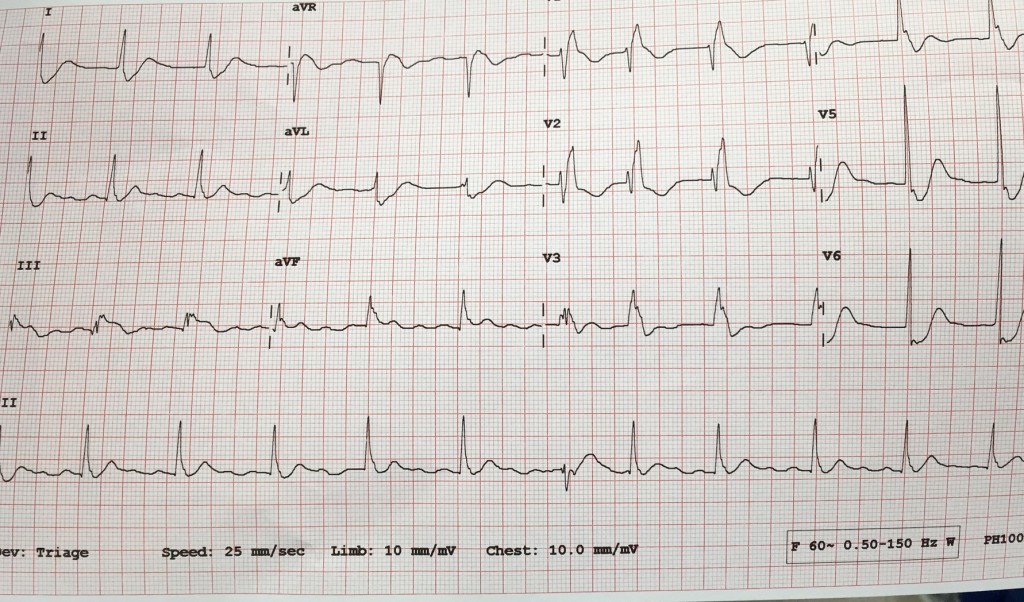
Anti-Arrhythmics
- Among the sodium channel blockers, they are divided into IA, IB and IC. Procainamide is the common IA, Lidocaine is a IB and Flecanide is IC
- Class II antiarrhythmics are the beta blockers
- Class III antiarrhythmics are K channel blockers. Amiodarone is the most common example
- Class IV antiarrhythmics are the Ca channel blockers
- Beta-blockers and calcium channel blockers should be used with caution in the setting of CHF exacerbation given their negative inotropic effects
- Amiodarone has both rate and rhythm-control properties
- Ibutilide and procainamide are the safest medications to give in the setting of WPW
- Dr Huecker: Can also consider adding magnesium to any of the aforementioned therapies
Infective Endocarditis
- Defined by the Modified Duke Criteria
- Most commonly caused by Staph species
- Don’t forget about pseudomonal coverage in those with prosthetic valves
- Valves are at high risk of infection given their lack of robust vasculature as well as the turbulent flow around them
- IE cases are increasing due to both increased IVDU as well as increased prosthetics being placed
- The average age of IE is now >65. Majority will require surgical intervention
- Recall Osler nodes, Janeway lesions, splinter hemorrhages, Roth spots/ conjunctival petechiae
- IVDU leads to right-sided IE
- When IE is diagnosed don’t forget to get blood cx from 3 separate sites
- Empirically give Vancomycin. Add on pseudomonal coverage if pt has a prosthetic valve
- The biggest RF for IE is prior IE
- Undomiciled patients are at increased risk of IE due to Bartonella species given flea exposure
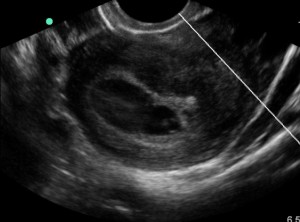
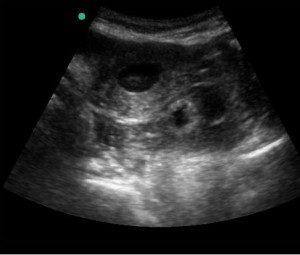
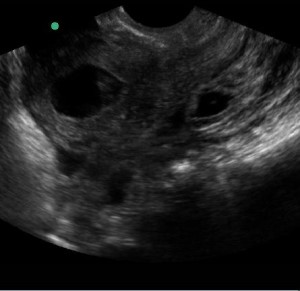
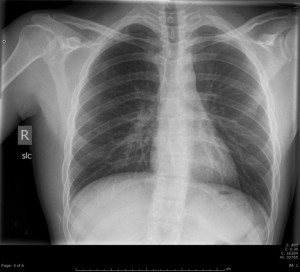
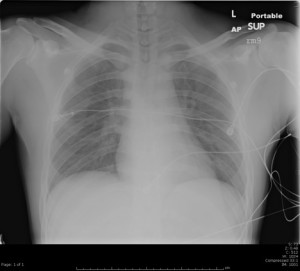
Ultrasound in the Unstable Patient
- CXR sensitivity for edema/ effusions is low
- Ultrasound has good sensitivity in confirming ETT placement
- Palpating pulses during ACLS has poor sensitivity/ specificity, another area where ultrasound can be helpful, in addition to checking for reversible causes of a patient’s arrest
- Ultrasound can be used to find the CO plus the SVR, which together can be very valuable information when resuscitating an undifferentiated shock/ SOA/ hypotensive patient
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)