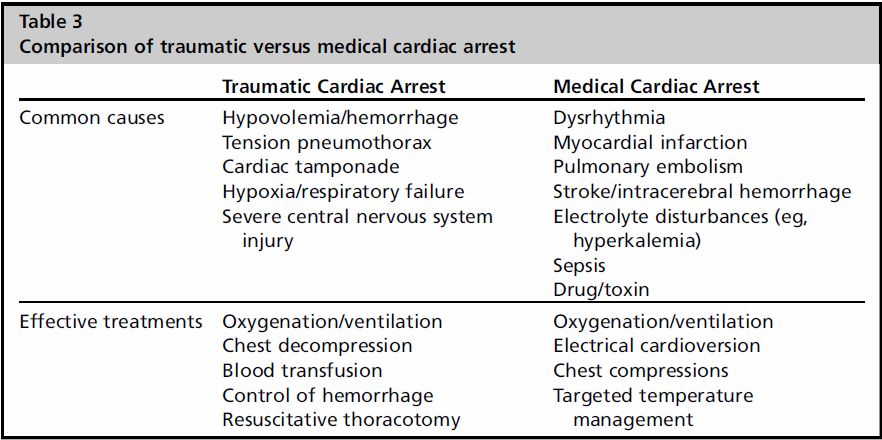
It’s trauma season once again. As room 9 after room 9 roll in the door the rising 2nd and 3rd years will soon be dealing with traumatic arrest patients (if they haven’t already). While the ED resident works to control the airway, the trauma team is placing bilateral chest tubes and a cordis. All of this while the nurses and techs continuously perform compressions and give 1mg of epi every 3-5 minutes, while inadvertently interrupting everything else going on. At the end of the day are all those compressions and all the epi going to change outcomes? We know in medical cardiac arrest it will but is traumatic cardiac arrest different?
Reanimating Patients After Traumatic Cardiac Arrest A Practical Approach Informed by Best Evidence discusses 5 key principles to guide management. The emphasize this is only for isolated traumatic cardiac arrests and that if there is any indication that a medical cardiac arrest occurred prior to a trauma following guidelines such as ACLS should be given priority.
The 5 Key Principles:
- Start or Stop
- Deprioritrize Chest Compressions
- Fix Ventilation
- Stop the Bleeding
- Fix the Physiology
Start or Stop:
When do you start or stop a traumatic resuscitation? What Factors do you consider? Well there is some food for thought:
Favorable Prognostics Factors:
- Penetrating injury, particularly to the Thorax
- Vitals Signs at any time
- Signs of Life at any time
- Short Duration (<10min)
- Cardiac Contractility on POC USN
Without 1 of these signs, survival is <1%. Important to keep in mind when EMS is giving a report and you are try to determine how long to attempt a resuscitation.
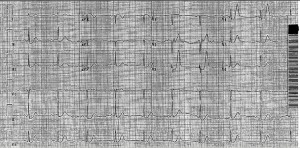
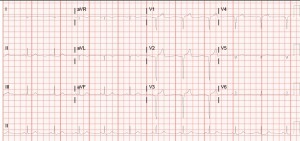
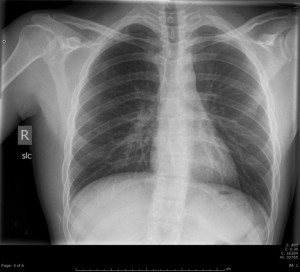
Spectrum of Output States:
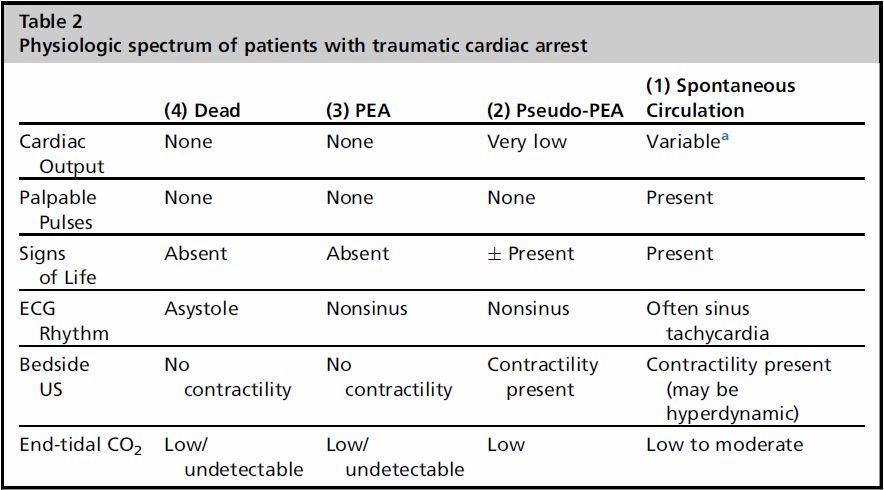
They note for their practice the category of “dead” does NOT receive any further resuscitation. The note this is in part to save the vital limited resource of blood prodcuts. I also found it interesting that they separate PEA from pseudo-PEA from severe hypovolemia. Thats why having the cardiac probe in hand on arrival can save be useful in determining how far you are going to push the resuscitation.
Deprioritize Chest Compressions
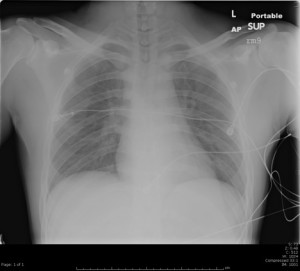
Chest compressions may work for medical arrest but the pathology behind traumatic arrest is so vastly different all they do is get in the way of more vital procedures: intubation, chest tubes, central access, cardiac USN. Until all this has been established it would probably be better just to hold compression. Be warned however this will likely be an uncomfortable experience for the nurses/techs.
Fix Ventilation:
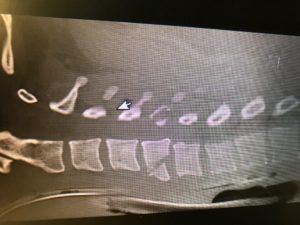
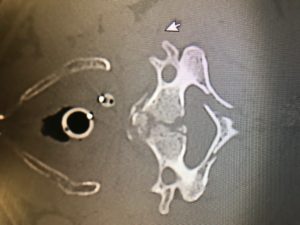
Referring back to Table 3 we can clearly see that establishing an airway and decompressing both sides of the chest should be top priority in a traumatic arrest.
Remember that traumatic arrests are a low flow state and while most patients while not require a induction agent or paralytic if you do use a paralytic use TWICE the dose.
Stop the Bleeding:
Simple and straight forward if it’s bleeding make it stop. Direct Pressure, tourniquets, topical hemostatic agents (which as far as I’m aware we don’t have) and pelvic binders are all easily performed in room 9. Thoracotomy is also something to consider discussing with Trauma early on in these resuscitations. Both the Eastern Association for the Surgery of Trauma and the Western Trauma Association recommend thoracotomy and though their conditions vary penetrating trauma to the torso and arrest for less than 15 minutes seems to be a good rule of thumb.
Fix the Physiology:
Pretty straightforward recommendations that we do everyday:
- Keep the Patient warm to prevent exacerbating coagulopathies
- Establish AccessL Large bore (14-18 gauge) IV access above the diaphragm, IO access of the proximal humerus, 8 or 9-Fr CVC preferably subclavian while avoiding multiple lumen CVCs
- Minimize fluids and transfuse blood products 1:1:1 and allow for permissive hypotension
They go into some post-resuscitation recommendations as well when it comes to “fix the physiology” but those are less important to use. I would recommend that everyone should briefly review this article as it has a lot more information and reasoning behind their recommendations.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)