I had a case in our department that I won’t forget for a while, and it reminded me to keep my differential broad even if the suspected diagnosis seems blatantly obvious.
An early 40’s female presented to our ER about 5 days after an MVC in which she was the restrained driver, where the car rolled onto its side going about 40s-50s MPH. + LOC, + airbags. Paramedics arrived on scene after a while when she was up and walking, and she refused to be taken to the ER. Over the following 5 days, she had near constant neck pain as well as a worsening headache and worsening abdominal and “rib” pain on the lower left side.
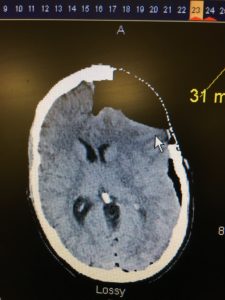
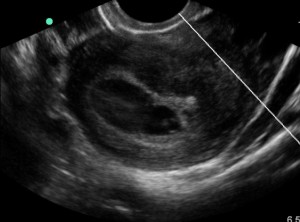
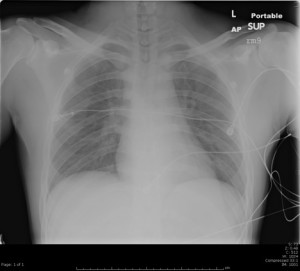
She presented to our ER in a hallway bed, where her initial HR was in the mid 80s, but BP was 80s/40s on multiple checks. O2 sat and temperature were normal. Mental status was normal, and there were no physical signs of trauma on her body. She had tenderness to the L lower and lateral ribs, as well as LUQ/LMQ abdominal tenderness, and lower midline C-spine tenderness. I quickly had her placed in a cervical collar, and brought the ultrasound to bedside a performed a FAST, which was negative (to my surprise).
I ordered fluid boluses, trauma labs, type and crossmatch, and planned to send her for a man scan, but her kidney function showed an AKI and therefore had to wait for one fluid bolus before going to the scanner. BP slowly started to trend upwards, not reaching over mid 90s systolic before she went to the scanner. Of note, she did have a slightly elevated white count in the mid-to-upper teens.
My differential? Trauma, trauma, trauma. She has to be bleeding somewhere, she may have a fractured C-spine, intracranial injury, intraabdominal injury, likely splenic laceration. My FAST just must not have picked it up. Given the history and clinical circumstance, I don’t think I was completely wrong for not having anything else on my differential for this hypotensive patient with concerning physical exam findings 5 days out from a serious car accident.
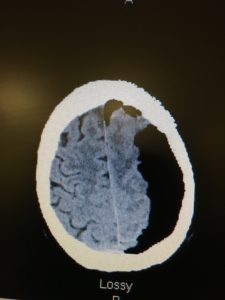
Once her man scan was done, I looked though the scans and noticed her right kidney was heterogenous with contrast enhancement with stranding around it. No fluid in her pelvis, and the rest of the man scan was entirely negative. Radiology soon called and said she had the “worst case of pyelonephritis I think I’ve ever seen”. A urine sample was finally collected after the scan resulted, which was, no longer to my surprise, infected. Upon talking to the patient, she denied any dysuria or frequency, but said her urine was “green” this morning. She never had any suprapubic pain.
That is the story of how I admitted a patient to medicine for pyelonephritis after getting a man scan and diagnosing it on CT. I don’t think I’ll be changing the top item on my differential, but I think I will keep other causes of hypotension and shock on my differential until they are ruled out in cases of delayed trauma presentation, such as this one.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)