Obstetrics and Gynecology Emergencies – Dr. Marques
Normal Vaginal Delivery Key Steps
- Support the perineum to prevent tearing with delivery of the anterior shoulder
- Upon delivery of the anterior shoulder, provide upward pressure to deliver the newborn
- Pull only gentle traction when delivering the placenta, to avoid uterine inversion
Post-Partum Hemorrhage
- Palpate the uterus to feel for inversion or retained products
- Provide tone by providing suprapubic pressure with an external hand and uterine pressure with an intravaginal hand
- Oxytocin can be given IM or IV to treat uterine atony
Shoulder Dystocia
- Leg hyperflexion and abduction at the hips along with suprapubic pressure (McRobert’s Maneuver) can be done if the anterior shoulder cannot be delivered
Breech Delivery
- This happens in 3-4% of all deliveries
- Do not pull traction at any time, as this can lead to entrapment in a cervix that is not dilated
- A pressure against the popliteal fossa can help flex the leg and deliver each leg
_____________________________________________________________________________
Oral Boards: Sepsis Due to Spontaneous Bacterial Peritonitis – Hugh, Shoff, MD
- The CMS Core Measures (SEP-1) provide quality measures for providers to follow in sepsis
- Severe Sepsis is defined as Lactate >2 or organ dysfunction
- Septic Shock is defined as severe sepsis with hypoperfusion despite fluid resuscitation or lactate>4
- Within 3 hours of presentation, obtain a lactate, blood cultures prior to broad spectrum antibiotics, and 30cc/kg fluid resuscitation
- Within 6 hours, lactate must be repeated if >2
_____________________________________________________________________________
CCU Follow-Up – Phil Giddings, MD
Myocardial bridging- coronary arteries travel deep into myocardium as opposed to laying upon the muscle
The vessels are occluded but when there is demand ischemia it can look like a STEMI
Myocardial bridging is fairly common in the general population, but usually isn’t symptomatic or pathologic.
If it is symptomatic- you could do Ca2+ channel blockers, beta blockers, and even myotomy or CABG if you’re feeling wild.
_____________________________________________________________________________
Urology Review- Isaac Shaw, MD
Priapism-
- Normal tumescence- veins constrict so the corpus cavernosum engorges because blood flows in
- Ischemic= low flow, less venous outflow, rigid, painful
- Nonsichemic= high flow, more arterial inflow, half rigid
- (Distinguish w/ a blood gas)
- Treatment
- anesthetize by blocking the dorsal nerve of the penis (2 & 10 o’clock) w/o epi
- then aspirate at 3 or 9 o’clock from the corpus cavernosum
- Use a phenylephrine stick from Room 9, 100mcg-500mcg Q1-5min
Fournier’s Gangrene
- polymicrobial
- assoc w/ DM
- 22-40% mortality
- empiric + clindamycin (clinda first because it’s addressing the toxins)
consult surgery before imaging
Paraphimosis
- foreskin trapped proximal to glans so the tip can get ischemic
- Treatment: manually reduce, dextrose, lube, may have to incise the dorsal foreskin
Phimosis
- foreskin can’t be retracted over the glans 2/2 inflammation
- Treatment in ED: topical steroids with urology follow-up
Urinary Retention
- often have hesitancy, nocturia, frequency, urgency
- >200cc PVR
- d/c w/ Foley à Uro will keep that in for 2 weeks prior to void trial
Renal Stones
- remember that 10-15% don’t have hematuria
- CT w/o contrast is still the standard for diagnosis, but some emergent literature exists that US alone is sufficient in young, healthy patients
- if <5mm, 90% pass; but if >8mm, 5% pass
- admit for intractable vomiting, pain, urinary extravasation, infection & obstruction
Balanitis
- Candida on the glans
- Associated with DM or uncircumcised
Torsion
- twisted around the spermatic cord
- if actively torsed, you will NOT have a cremasteric reflex
- ultrasound 88-100% sensitive because they can torse and untorse
- consult before imaging
_____________________________________________________________________________
Breaking Bad News– Frank Woggon, PhD
- insensitive truth telling can have similar effects as lying
- goals include gathering info, provide info, support patient, strategy for care
- keep it simple, no jargon, talk slow, repeat PRN, use neutral language, be honest, allow emotions, consider cultural differences
- “compassion is the willingness to let yourself be affected by the life and suffering of others”
SPIKES
- Setting- privacy, sit down, eye contact, turn off pager
- Perception- don’t combat denial at first, interpret first
- Invitation- ask how much they want to know first
- Knowledge- “what I’m about to say is not good,” be direct but not blunt, use their language
- Empathize- ok to validate the emotions, silence is ok
- Strategy & Summary- what comes next
GRIEV_ING Protocol
- Gather the family
- Resources- call for support
- Identify yourself & staff, those in the room
- Educate the family about what happened
- Verify that the patient died by using that word
- SPACE- silence is ok, let them have their gut reaction
- Inquire whether they have questions
- Nuts & bolts- organ donation, funeral arrangements, personal belongings, etc.
- Give contact info for f/u questions
_____________________________________________________________________________
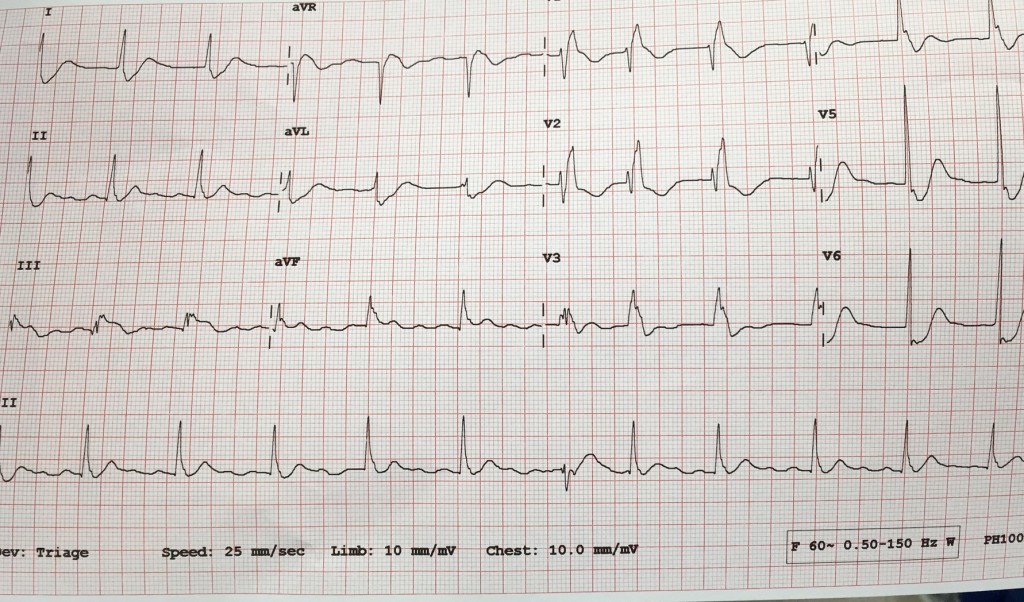
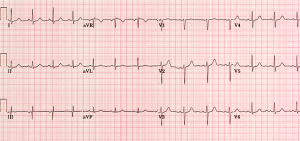
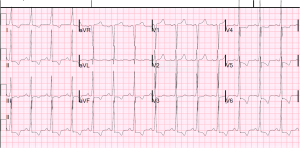
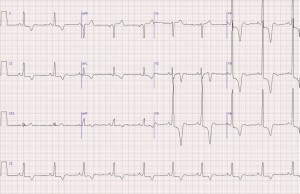
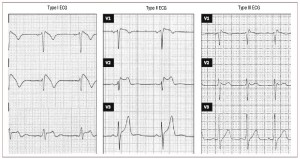
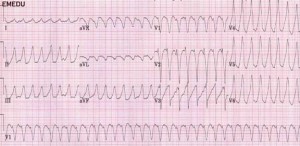
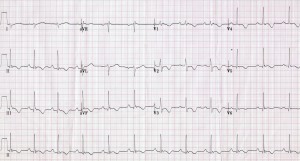
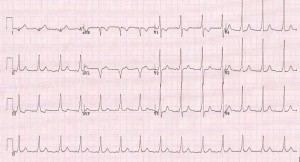
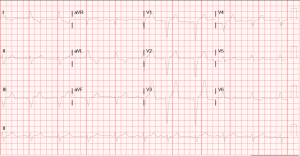
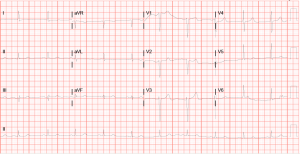
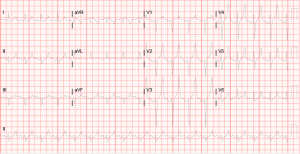
STEMI Mimicks – Frank Shary, MD
OMI= occlusive MI
- V2 & V3 2mm elev = STEMI; Everywhere else 1mm
- Wellens: biphasic T wave, they recently had an OMI, symptoms may have gotten somewhat better by the time of the EKG, they need a cath
- Deep T Wellens- deep and wide
- LV aneurysm- deep Q wave w/ biphasic T wave, static
- Sgarbossa criteria- OMI in the setting of LBBB and/or paced rhythm
- look at vector of QRS and vector of ST segment
- concordant elevation or depression greater than 1mm
- discordant greater than 5mm
- Hyperacute T waves- early into the ischemia, before ST elevation, cath soon because you have potential to save more myocardium, large area under the curve especially in proportion to the QRS complex
- L circumflex is the vessel most likely to be silent
- aVR- if it’s the only lead elevated and everywhere else is diffusely depressed, you might have diffuse subendocardial ischemia
- could be bad triple vessel disease
_____________________________________________________________________________
Managing the Bleeding Patient Without Blood Products – Chase, PharmD
There are 6 Jehovah’s Witness churches in Louisville
- Plasma Derivatives are technically not Blood products… so whether or not a patient wants that is up to the individual
- albumin, clotting factors, PCC, Immunoglobulins (including Rhogam and vaccines)
- equine Ig and Crofab could also be iffy
- ECMO, cardiopulmonary bypass, dialysis are allowed generally
Source Control
- bone wax/putty- use in NES and long bone fx, high infection rate though
- oxidized regenerated cellulose- ex. Surgicell, promotes rebuilding of proteins to heal & achieve hemostasis, like a mesh
- gelatin matrix- ex. Floseal, more like a gel
- there is a powder too but it’s $$$ and causes microemboli so don’t use
- thombin- apply w/ 4×4’s
- TXA- derivative of lysine THIS IS NOT A PLASMA DERIVATIVE SO THEY SHOULD BE OK WITH IT, 1g over 10min à another 1g over 8-10 hours
- have a lower threshold to give TXA since there is a decrease in mortality, even if you wouldn’t have given TXA to a non-Jehovah’s witness
Usable Therapies:
- Cell Saver
- blood is collected, washed, centrifuged, returned to patient
- example indications: AAA, TKA, THA, cardiac surgeries
- Vitamin K
- PCC- most efficacious
- 4 factor is better than 3 factor, but if you try to give 3 factor and then just add Factor VII a la carte, more thromboembolic events
- FFP- prep time is longer, tonzo volume
- Adnexanet Alpha- new antidote for rivaroxaban and apixaban, we don’t have that
- Novo7- directly activates Factor VIII, black box warning for thromboembolic events, no difference in mortality but there was a reduction in transfusions
- Dabigatran reversal- idarucizumab, dialysis, charcoal
- Antiplatelet reversal- ASA and Plavix are irreversible, but ticagrelor is reversible
- DDAVP- indicated for DI, von Willebrand disease, uremic bleeding (renal failure), nocturnal enuresis
- 0.4mcg/kg over 10min
_____________________________________________________________________________
Pediatric Environmental Emergencies- Dr. Said
Drowning
- fresh or salt water doesn’t matter, you’re ruining your surfactant
- if you are anoxic you get brain damage in 4-6min, irreversible
- cold temp is only helpful if it happens really quickly
- outcomes depend on initial resuscitation, degree of pulmonary damage, time submerged
- poor prognosis- coma, apnea, submersion >9min
- can try vapotherm for positive pressure, albuterol can treat bronchospasm
- steroids don’t help
- goal warming 32C
- if asymptomatic, obs for 8 hours! Oy vey
- admit if prolonged submersion, respiratory or neuro symptoms, abnormal CXR
Electrical Injuries
- lightning strikes carry 30% mortality risk, it causes asystole
- doesn’t cause renal failure or burns/compartment syndrome
- thicker tissue less damaged
- tissue between entry and exit wounds could be more damaged interiorly than it appears
- AC worse than DC because AC at low voltage causes tetany so you’re holding on longer
- we use DC for defib, countershock, pacing but you get thrown off
- oral electrical injury – monitor for progressive edema
- could have delayed bleeding from labial artery
_____________________________________________________________________________
EMTALA- Melissa Platt, MD
- in court, all are case-by-case
- we have to provide a medical screening exam and treat and stabilize an emergency medical condition
- transferring physician assumes the risk if the patient crumps en route to accepting hospital
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)