From Dr Faryar
Journal Club February 2014
The Cunningham Technique
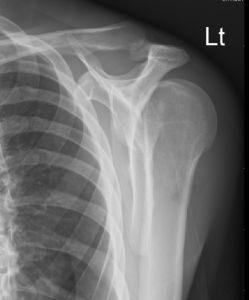
Young male with history of psychiatric illness and seizures presents with left arm pain after a fall. Patient thinks he slipped on ice, but is unsure. He reports no LOC, no head pain, no neck pain. Does not believe he had a seizure. No urinary incontinence, no tongue biting. Has severe pain in left shoulder. Physical exam shows small forehead abrasion, no c-spine tenderness, and decreased ROM to left shoulder. He holds his arm internally rotated and adducted. There is an obvious deformity to the left shoulder with a defected palpated anterior.
3 view x rays ordered in triage read as negative for fracture or dislocation, but limited by poor patient positioning.
I was pretty sure that it was dislocated, so I went ahead and ordered the definitive axillary view.
As I was charting on another patient, the x-ray tech came over, looking slightly embarrassed, and said that she was pretty sure she had just reduced my patient’s shoulder as she was trying to get him in the proper position for the axillary view. She said, “It was amazing, he couldn’t move it, then pop, and he has full ROM now.”
Nice.
Two minutes later, got a phone call from radiology…Might have missed a posterior dislocation…Looks great in the axillary view now…Would recommend getting repeat normal films to be sure that there was no fracture missed while it was not in proper position.
Ordered the repeat 3 view x-rays and went to make sure he was still reduced. Found my patient still internally rotated, in pain, not able to move, and still with the hollow anteriorly. Gently held his hand and arm and before he realized what I had done, pulled slightly and externally rotated and put it back in place. As I called for the sling, he went to take his gown off and it slid back out as he extended his arm and moved it anteriorly. Tried again to gently externally rotate it, but he was now on to me and and was tense and pulling against me. Asked for suggestions other than sedation and got one from the one and only Dr. Martin Huecker: Try the Cunningham technique.
I went back in his room. He was looking a little wary. I told him it’s not going to hurt; I was just going to massage his arm a little bit to see if it will go back in. I held his left forearm in my left hand at the elbow and, using my right hand, massaged first his trapezius, then his deltoid, then his biceps, then his deltoid, then his trapezius, then his deltoid ….annnnnnnnnnnnd….. it slid back in place. Patient looked as surprised as I did. Immediately put him in a sling and swathe. Got repeat x-rays in the sling.
He was in the department for about 30 minutes after that while awaiting x-ray reads and his arm stayed reduced while in the splint. No fractures on x-ray. He was discharged with orthopedic follow up in the sling.
One can find is a formal description of The Cunningham technique from the blog “Life in the Fast Lane.” http://lifeinthefastlane.com/cunninghams-shoulder-relocation/
- Inform the patient of the procedure and the fact that it will be painless. It is important to relax the patient and confident reassurance is the first step towards this.
- Sit the patient up with the back vertical. This can be done on a bed, chair or trolley, but preferably seated on a non-wheeled chair without arm rests.
- Carefully support the arm while it is moved into the correct position, allowing the patient to help with the other arm. The correct position is with the arm adducted (next to the body) and pointing vertically down, the elbow is flexed at 90 degrees so that the forearm points horizontally and anteriorly.
- The operator then squats/kneels to the side of the patient and facing the opposite direction to the patient. The operator then slips the hand between the patients forearm and body so that the patient’s wrist/hand is resting on the operator’s upper arm. Do not make pulling movements at any time as this will elicit pain and result in spasm.
- Apply steady, very gentle traction (the weight of the operators forearm is quite enough) directly downwards once the patient is settled and pain free. Keep this gentle weight on the arm throughout, stop if any spasm or pain. Usually resting with the patients arm in this position will start to reduce the pain of spasm.
- With the other hand, the operator then massages the trapezius, deltoid and biceps muscle sequentially, repeating this process and concentrating on the biceps brachii until the muscles are fully relaxed. A strong kneading of the biceps with the thumb anterior and the four fingers of the operator posterior to the arm is recommended. At this point the humeral head will relocate usually without any clear indication that the shoulder has reduced (no sound or ‘clunk’ feeling). This means that the shoulder must be observed/checked regularly to confirm when relocation has occurred (with shoulder exposed movement can be seen as the ‘step’ disappears.)
And a link to the blog with the description. It has a nice video.
The Wonder of Ultrasound
Great case I had in December. Overall good month, but this case was especially interesting, and humbling. It combines the excitement of chest pain, the enigma that is leg weakness, and humbling realization of a life threatening diagnosis.
Working in the ED one day and the psychiatry intern goes to see a patient. Routine patient, who had presented with right leg tingling and weakness that made it all the way to the back of the ED. Bed 15. Basic labs pre-ordered as well as a chest X-ray for a brief episode of chest pain that the patient told triage. Of course, the sixth vital sign, an ekg. Intern is with the patient for about 5 minutes and returns. He tells me that he is concerned that the patient is sick and wants me to see the patient sooner than later. He is concerned for possible stroke due to right leg weakness and pain. I tell him of course and I go see the patient.
HPI: 58 y/o AAM with hx of seizures on Dilantin but no other medications or PMH presents with chief complaint of right lower leg pain and tingling. Patient states that while at work today, he was lifting boxes and felt a sharp chest pain that started in the middle of his chest and radiated to between his shoulder blades. It then shot to his pelvis and went away. He went back to work for about 10 minutes then started to have right leg pain. He tried to drive to the hospital, but had to stop and call an ambulance due to sever RLE pain. All other symptoms had resolved at this point. No n/v, diaphoresis, dizziness, loss of bowel or bladder.
Pertinent Hx: NKDA, 30yr pack hx of smoking, dilantin.
Vitals: BP: 148/62, HR 66, RR 18, O2 100% T 98.5
Significant Physical Exam –
RRR, no m/r/g, CTAB, abd soft, nt, nd, no bruit, no pulsating mass
RLE strength 4/5, LLE 5/5.
No DP, PT, popliteal, or femoral pulse in the right leg.
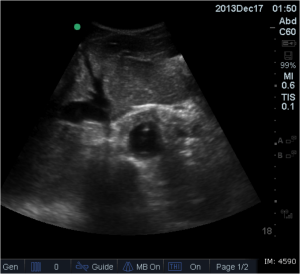
At this point I was concerned. I excused myself and got the bedside ultrasound. In my head I wondered was this just a arterial occlusion, or was this something greater?
Well this is when I started to sweat. I tell the patient what I think my diagnosis is, and head back to my desk to get orders going. At this time I review the labs and chest X-ray.
CBC – WNL, CMP – K 3.3, UA WNL, Troponin Neg, Tox Screen Neg, Coags neg.
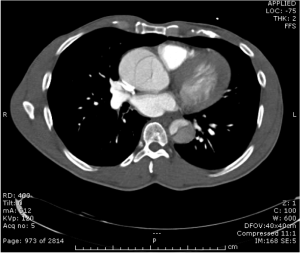
Chest Xray –
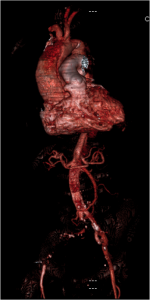
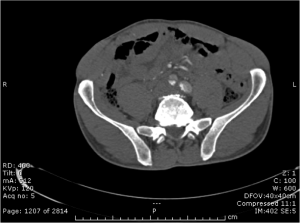
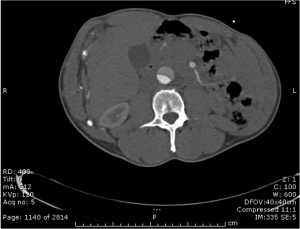
Any more concern? At this point I ordered a CTA of the Chest/Abdomen/Pelvis as well as called the surgery team. I wanted to get them involved early in the case that the patient deteriorates. I assessed the patients blood pressure at at the time was 130/60 and HR 58. I got the nurse to get the patient to the CT scanner as well as discussed with the trauma team. At this time patient had stable vital signs and pain controlled with morphine. Trauma evaluated and the CT resulted.
We now have our diagnosis. When patient got back from CT scanner, his blood pressure was increasing and now 150/80 and HR 68 with increasing pain.
Esmolol gtt was started, arterial line place, and the patient was transferred to another local hospital to undergo cardio-thoracic surgery for repair.
Diagnosis – Aortic Dissection from the level of the aortic valve down through the bifurcation of the iliac arteries. From the one slice, you can see he had no flow to the right leg. CTA demonstrated some collateral from the gastrics, but overall no flow.
Patient outcome – survived surgery. Otherwise have not been able to follow-up past that time. I shared this case because I feel it is a good representation of a case where easy bedside diagnostics can give you the diagnosis early and lead to your diagnosis. With the chest X-ray as well as the bedside ultrasound, we knew what the patient had. The CTA was just icing on the cake. Never be afraid to use the ultrasound. If it had been negative, this could have gone a completely different direction. Credit to the psychiatry resident for getting me involved early.
Use the ultrasound. Use it early. Diagnose early.
Social Media
Paucis Verbis
Academic Life in Emergency Medicine (ALiEM) has 128 “Paucis Verbis” (in few words, brevity) cards, which are PDF files that are mostly 1 page each, that have quick info on many of the issues we’ll see in the ER.
With DropBox, or something like it, it’s a great way to look up quick hitters.
On the Medicolegal tip
I love these articles that scare the crap out of me. Took some navigating to get this pdf and it looks like the unofficial manuscript. Saw it on EM Lit of Note. Another good one of his was the EMR exposing one. 28% patient care, 44% data entry. We are drones.
FOAMed Lecture
Here is the ppt file from lecture. Again most of the links are on Room9ER homepage. LEt me know if you have any further interest.
Hope to start posting all powerpoints and or the audio / ppt tegrity files once I come on in Nov.
FOAMed
Hey here is a great set of slides, similar to my FOAM presentation. This was posted just hours after my lecture.
www.slideshare.net/DavidMarcus3/foam-primer-stony-brook
Back pain
How often is this in our differential? I have to admit, not very often in mine.
This article from UpToDate discusses vertebral osteomyelitis/discitis.
Have a good day, everyone.
January Admin Project
Most of you that have done admin work or paid attention to trends in DED, you probably have noticed that many months the majority of deaths in the ED stem from catastrophic brain damage, from both traumatic or spontaneous causes. Over 80% of my DED’s were related to severe neuro injury, so I looked at some of our common practices in handling head injuries and spontaneous bleeds and very quickly noticed that we don’t really follow any consistent patterns in caring for these folks.
Many of these patients have non-survivable injuries no matter what we do, however there are some simple interventions that might be beneficial to some cases. For instance, elevating the head of the bed >30 deg (but not more than 40) can drop ICP by 8-10mmHg, and loosening or removing an unnecessary c-collar can actually further decrease ICP by 2-5 mmHg. These are all evidence based, and while only effecting small changes, could help improve some patient’s outcomes. In addition, in discussing this with Neurosurg faculty and looking at the literature, our practice of pre-medicating head injury patients with Lidocaine is based on an old, underpowered and poorly applicable study, that used only 20 patients with known brain tumors, and is really not proven or necessary.
The following are some suggestions in dealing with Neurosurgical cases. These are practice parameters, and should be considered with every case, but this is not something that will be made standard of care, as each case should be handled appropriately at the individual physician’s discretion. However, if these interventions are not implemented, Dr. Coleman and Dr. Nauta both recommended documenting your rationale in your MDM. Also, the studies that support these practices, and some of the poorly done studies that are the basis for some of our current practices, are listed.
Increased Intracranial Pressure Protocol
Level 1
Elevate Head of Bed (30 – 40°)
Check C-collar Fit, remove as soon as possible (can ↓ ICP 2 – 5 mm/Hg, collar not necessary in isolated GSW to head, and coexistent c-spine injury rare)
Temp Normal (maintain < 98.0°F)
PaCO2 35-38 mmHg (based on EtCO2 or ABG)
Control Pain/Sedation Package if Intubated (Fentanyl)
Pre-intubation Lidocaine (100mg IV) only if known tumor
Urgent Neuro Imaging
Ocular Ultrasound (Optional, do not delay definitive imaging)
Level 2 – Perform in conjunction with NES consult
Osmotic Therapy*
Mannitol – 1g/kg over 10 minutes (if hypertensive)**
Hypertonic Saline 3% – 250mL over 10 – 15 minutes (if normo or hypotensive)***
Sodium Bicarb (2 amps over 10 minutes)****
Foley catheter, replace fluid losses
Normal Saline 0.9% (No LR, D51/2NS, etc.)
Maintain Na ~ 150
Phenytoin load (15 – 20 mg/kg) only in patients with seizure or posturing
Steroids only in the case of known tumor
*Normal physiologic osmolarity range is approximately 280 to 310 mOsmol/L.
**Osmolarity of Mannitol is 550 mOsmol/L.
***Osmolarity of 3% saline is 1027 mOsmol/L
****Osmolarity of 2 amps NaHCO3 in NS is 1790 mOsmol/L
Level 3 – Perform in conjunction with NES consult, requires ICP monitoring
Propofol (or Phenobarb) gtt titrated to low levels of sedation scales (50-200 mcg/kg/min)
BIS monitoring
CPP Optimization (CPP= MAP – ICP) greater than 55 – 60
Level 4 – Only NES/NeuroAnesthesia applicable
Decompressive Craniectomy
Induced Hypothermia
Pentobarb coma (burst suppression)
Moderate Hyperventilation (Reserved as temporizing measure for patients actively herniating)
HOB
Feldman Z, Kanter MJ, Robertson CS, et al. Effect of head elevation on ICP, CPP, and CBF in head-injured patients. J Neurosurgery. 1992;76:207-211.
Ng I, Lim J, Wong HB. Effects of head posture on cerebral hemodynamics: its influences on intracranial pressure, cerebral perfusion pressure, and cerebral oxygenation. Neurosurg.2004;54:593-598.
Rosner MJ, Coley IB. Cerebral perfusion pressure, intracranial pressure, and head elevation. J Neurosurg. 1986;65:636-641.
Moraine JJ, Berre J, Melot C. Is cerebral perfusion pressure a major determinant of cerebral blood flow during head elevation in comatose patients with severe intracranial lesions? J Neurosurgery. 2000;92:606-614.
C-Collar
Stone MB, Tubridy CM, Curran R. The effect of rigid cervical collars on internal jugular vein dimensions. Acad Emerg Med. 2010 Jan;17(1):100-2.
Mobbs RJ, Stoodley MA, Fuller J. Effect of cervical hard collar on intracranial pressure after head injury. Aust J Surg. 2002 Jun;72(6):389-91.
Temp
Shiozaki T, Hayakata Taneda M, et al. A multicenter prospective randomized trial of the efficacy of mild hypothermia for severely head injured patients with low intracranial pressure.JNeurosurg. 2001;94:50-54.
Clifton GL, Miller ER, Choi SC, et al. Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med. 2001;344:556-563.
Metz C, Holzschuh M, Bein T, Woertgen C, et al. Moderate hypothermia in patients with severe head injury: cerebral and extracerebral effects. J Neurosurg. 1996;85:533-541.
Marion, DW, Penrod, LE, Kelsey, SF, et al. Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med. 1997; 336:540-546.
Polderman KH, Joe RTT, Peerdeman SM, Vandertop WP, Girbes ARJ. Effects of therapeutic hypothermia on intracranial pressure and outcome in patients with severe head injury. Intensive Care Med. 2002;28:1563-1573.
Resp Rate
Muizelaar JP, Marmarou A, Ward JD, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75:731-739.
Newell DW, Weber JP, Watson R, Aaslid R, Winn HR. Effect of transient moderate hyperventilation on dynamic cerebral autoregulation after severe head injury. Neurosurg.1996;39:35-43.
Diringer MN, Yundt K, Videen, TO, et al. No reduction in cerebral metabolism as a result of early moderate hyperventilation following severe traumatic brain injury. J Neurosurg. 2000;92:7-13.
Muizelaar JP, Van Der Poel H, Li Z, Kontos HA, Levasseur JE. Pial arteriolar vessel diameter and CO2 reactivity during prolonged hyperventilation in the rabbit. J Neurosurg. 1988;69:923-927.
Osmotics
Smith HP, Kelly DL, McWhorter JM, Armstrong D, et al. Comparison of mannitol regimens in patients with severe head injury undergoing intracranial monitoring. J Neurosurg. 1986;65:820-824.
Khanna S, Davis D, Peterson B, et al. Use of hypertonic saline in the treatment of severe refractory post traumatic intracranial hypertension in pediatric traumatic brain injury. Crit Care Med. 2000;28:1144-1150.
Peterson B, Khanna S, Fischer B, Marshall L. Prolonged hypernatremia controls elevated ICP in head-injured pediatric patients. Crit Care Med. 2000;28:1136-1143.
Simma B, Burger R, Falk M, et al. A prospective randomized, and controlled study of fluid management in children with severe head injury: lactated ringer’s solution versus hypertonic saline. Crit Care Med. 1998;26:1265-1270.
Doyle JA, Davis DP, Hoyt DB. The use of hypertonic saline in the treatment of traumatic brain injury. J Trauma. 2001;50:367-383.
Quereshi AI, Suarez JI, Bhardwaj A. Malignant cerebral edema in patients with hypertensive intracerebral hemorrhage associated with hypertonic saline infusion: a rebound phenomenon? J Neurosurg Anesthesiol. 1998; 10:188-192.
Sedation and Paralysis
Hsaing JK, Chestnut RM, Crisp CB, et al. Early, routine paralysis for intracranial pressure control in severe head injury: is it necessary. Crit Care Med. 1994;22:1471-1476.
Temkin NR, Dikmen SS, Wilensky AJ. et al. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med. 1990;323:497-502.
Pittman T, Bucholz R, Williams D. Efficacy of barbiturates in the treatment of resistant intracranial hypertension in severely head injured children. Pediatr Neurosci. 1989;15:13-17.
Goodman JC, Valadka AB, Gopinpath SP, et al. Lactate and excitatory amino acids measured by microdialysis are decreased by pentobarbital coma in head-injured patients. J Neurotrauma. 1996;13:549-556.
Ward JD, Becker DP, Miller JD, et al. Failure of prophylactic barbiturate coma in treatment of severe head injury. J Neurosurg. 1985;62:383-388.
Cruz J. Adverse effects of pentobarbital on cerebral venous oxygenation of comatose patients with acute traumatic brain swelling: relationship to outcome. J Neurosurg.1996;85:758-761.
Disconnect
Stumbled upon this article on Twitter by “Skeptical Scalpel,” a surgeon in academic facility. This article was published in a surgical bulletin. The perspective of a plaintiff attorney. Interesting reading.
Dimer wins again
Here is a post from Ryan Radecki at EM Lit of Note. His philosophy mirrors what I took from Jeff Kline the PE guru on the approach to PE workup. When you have committed to ordering a CT-PA, then get a d dimer and if NEG, CANCEL the CT. Controversial of course. But the dimer is MORE SENSITIVE than a CT. Some say the d dimer is only for “low risk” patients, but check out this study using not necessarily low risk patients.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)