We have noticed more and more this culture in our ED of obtaining an initial ECG, an initial troponin, and then waiting 2 or 3 or 6 hours to obtain a second troponin only and then discharge if negative.
I dove into the literature and wrote this post to address the SECOND ECG AT TIME OF SECOND TROPONIN as part of a rule out strategy for low risk ED patients.
I will not even address the fact that people are not obtaining a 2nd ECG at time 20-30 minutes from the first. This is on UpToDate, in ACC guidelines, in ACEP guidelines. It is simply standard of care to obtain an early, repeat ECG on anyone you remotely suspect of having ACS. I harp on this in lectures and have posted on it before. I also will not be talking about hs-Troponin (high sensitivity troponin). Many articles and FOAMed commentaries have covered hs-Trop, and we do not have this test at UL. So please do not think you can rule out all comers with 1 troponin, because you need the hs-trop to even consider this.
This post relates to the issue of a repeat ECG at time 2hr or 3hr (I am not a 6 hour guy, I like the 2 or 3 hr depending on symptom time frame). Don and I discussed the 2nd ECG phenomenon and he said it is just our culture at UofL, hence inspring our Room9ER post. Well we need to change the culture.
Now I didn’t want Geralds to cherry-pick an article to try to rebut me on this, so I went down a rabbit hole of ACS rule out, nSTEMI, HEARTS, TIMI and cardiac markers.
If your attention span is reaching its limit here is the bottom line:
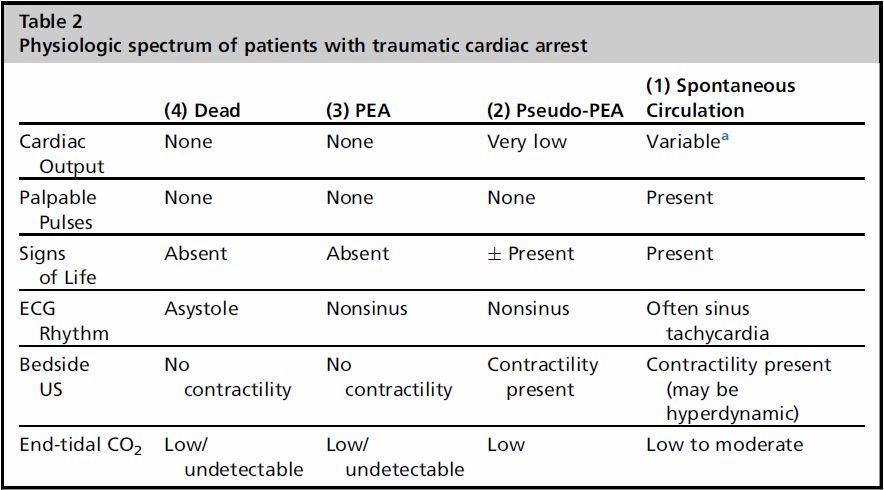
All rapid rule out tools and their validation studies involve at least a SECOND ECG with the repeat troponin. HEARTS, ACC/AHS guidelines, TIMI-based rule outs, etc.
I was early to drop the CK and CK-MB on initial and repeat marker testing in favor of solely the troponin, but dropping the ECG is irresponsible. And is not evidence-based.
Below are many quotes and a figure, then a letter to the editor, from various sources. It was actually somewhat difficult to find in the methods exactly when or even if a repeat ECG was done. Much of the time, the ECG done at time of 2nd trop was not even the 2nd ECG, as mentioned above. “Serial ECGs” is the rule. It seemed as though the repeat ECG(s) were implied in the study, and that the research question was simply timing a troponin.
Dr Huecker composed most of this post because Dr Bertolotti is so excited about and diligently preparing for Research Day.
Enjoy, and please post comments!
— Patients with probable or possible ACS but whose initial 12-lead ECG and cardiac biomarker levels are normal should be observed in a facility with cardiac monitoring (e.g., chest pain unit or hospital telemetry ward), and repeat ECG (or continuous 12-lead ECG monitoring) and repeat cardiac biomarker measurement(s) should be obtained at predetermined, specified time intervals (see Section 2.2.8). (Level of Evidence: B)
— The c-statistic of troponin only was 0.70. With addition of the ECG the c-statistic improved significantly to a value 0.78, with a likelihood ration test p-value of <0.001
— Anderson et al. JACC Vol. 50, No. 7, 2007 ACC/AHA UA/NSTEMI Guideline Revision August 14, 2007:e1–157 If the initial ECG is not diagnostic but the patient remains symptomatic and there is high clinical suspicion for ACS, serial ECGs, initially at 15- to 30-min intervals, should be performed to detect the potential for development of ST-segment elevation or depression. (Level of Evidence: B)
— ACEP (What will be used for or against you in court, as the case may be)
Acute Coronary Syndromes (Non–ST-Segment Elevation – Adult)
Critical Issues in the Evaluation and Management of Adult Patients with Non–ST-Segment Elevation Acute Coronary Syndromes (September 2006)
Complete Clinical Policy on Non–ST-Segment Elevation Acute Coronary Syndromes (PDF)
Scope of Application. This guideline is intended for physicians working in hospital-based emergency departments (EDs) or chest pain evaluation units.
Inclusion Criteria. This guideline is intended for adult patients presenting to the ED with suspected non–ST-segment elevation acute coronary syndromes.
Exclusion Criteria. This guideline is not intended for pediatric patients, patients in cardiogenic shock, or patients with injury on the initial 12-lead electrocardiogram (ECG).
Critical Questions
- Are serial ECGs useful during the ED evaluation of patients with suspected acute coronary syndromes?
- Level A recommendations. None specified.
- Level B recommendations.Perform repeat ECG or automated serial ECGs during the ED evaluation of patients in whom the initial ECG is nondiagnostic for injury and who have symptoms consistent with ongoing or recurrent ischemia. No recommendations can be made in regards to the exact timing of repeat ECGs. Studies suggest that 30 to 60 minutes after baseline may be a reasonable time interval for repeat ECG.
- Level C recommendations. None specified.
— Letter: Re: “Troponin-negative chest pain”—a diagnostic evasion?
This brief article is well written and I agree the diagnostic label of ‘troponin negative chest pain’ is unhelpful. However the article repeats some common misconceptions which require correction.
Firstly, the article implies that the majority of patients attending hospital with chest pain have an acute coronary syndrome. This is absolutely not the case – in fact most patients with suspected acute coronary syndrome do not have it. (1) Often patients receive a label of acute coronary syndrome and this is later corrected by the cardiology registrar or consultant on call – although by then it may be too late to change the patient’s perception that they have ‘had a heart attack’.
Secondly, there appears to be a misunderstanding of the value of troponin testing. Troponin assays are positive when there has been myocardial necrosis. They do not give any information about the mechanism of myocardial necrosis – a positive troponin can indicate acute coronary syndrome, but may also occur in heart failure, prolonged arrhythmia, sepsis, pulmonary embolism and many other situations. (2)
Similarly, a negative troponin does not absolutely exclude a cardiac cause for symptoms – nor does it mean the patient is necessarily in a low risk group. (3) Patients with unstable angina, dynamic ECG changes, but negative troponin should be considered as having a similar risk of mortality and morbidity to those with a normal ECG but a positive troponin.
Troponin assays should generally be considered a prognostic, not a diagnostic test, and should be used in conjunction with the patients history and ECG – never alone.
![]()
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)