Here is the Micronutrient Wellness lecture.
Author Archives: Martin Huecker
How Evidence Based Are We?
Here is a pretty comical article by Dr Ioannidis. If you do not know who this is stop now and read this.
This article was just published. It is written as a report to the father of evidence based medicine, Dr David Sackett. It takes a not terribly optimistic view of the current state of medical research. He calls out industry bias, ghost authorship, and many other flaws of our system. We are very lucky to have people like Dr Ioannidis ensuring integrity to the research process.
Managing Migraine
As mentioned on R and R in the Fast Lane. This article by Friedman is a welcomed update to evidence-based migraine management. Some people love treating migraine patients, some hate it. But we all have our cocktails we believe in.
I am a fioricet/neurontin/IM compazine, escalating to IV compazine/benadryl/decadron/toradol OR if they want to drive home IV MAG/decadron/toradol … kind of guy.
This article starts with criteria for delineating migraine from other headache forms. Then provides a succinct algorithm for treatment, starting with reglan or compazine +/- benadryl, then another dose plus toradol, then dihydroergotamine, then occipital nerve blocks (very fun), then as a last resort, opioids. I would encourage you to attempt a few other methods before the blocks and especially before the opioids.
Many other medications can be used (keppra, depakote, propofol, etc). But this is a solid overview of the EM approach. Also of note, see the Oct 2016 EM-RAP paper chase of the reglan +/- IV fluids in migraine article which showed no real benefit to the addition of IVF.
Stop Traffic
Hey guys some of you were lucky enough to hear my friend Olivia Mittel and her guests educate our group in didactics. She presented information on human trafficking. This is a real issue and many of us have likely discharged a trafficking victim back into a terrible situation. Please read this Annals of EM article for more information very relevant to EM doctors.
Hydration
The how to stay healthy in EM posts on Aliem are definitely worth checking out. One common piece of advice given on tolerating the night shift is hydration. Here is a cool study proving this, many studies like this in the literature.
Lactate
Bosse’s favorite molecule (and lab test), lactate has a sordid and confusing history. This article in Emergency Medicine News sheds some light on lactate and its role in disease (or health). The author (Dr Paul Marik) is board certified in internal medicine, critical care, neuro-critical care and nutrition.
It may take a couple reads but this article has a succinct, common sense approach to understanding lactate production and use by the body. You may not be able to apply this knowledge on your next patient encounter, but physiology is fun right?
Research Lectures
Just this month, the UL ID department presented lectures on research methods from the beginning to the end of the research process.
Louisville Lectures has posted the first 3 of them and they are fantastic as expected. Louisvillelectures.org continues to receive praise from Lifeinthefastlane blog. You can find the lectures on Youtube or iTunes as well.
Here is a link directly to the site, they are video lectures so I would recommend watching on this link, though if you like to listen while driving check podcasts on iTunes.
The lectures are brief enough to be valuable for all residents and faculty, worth repeated views for anyone interested in academics.
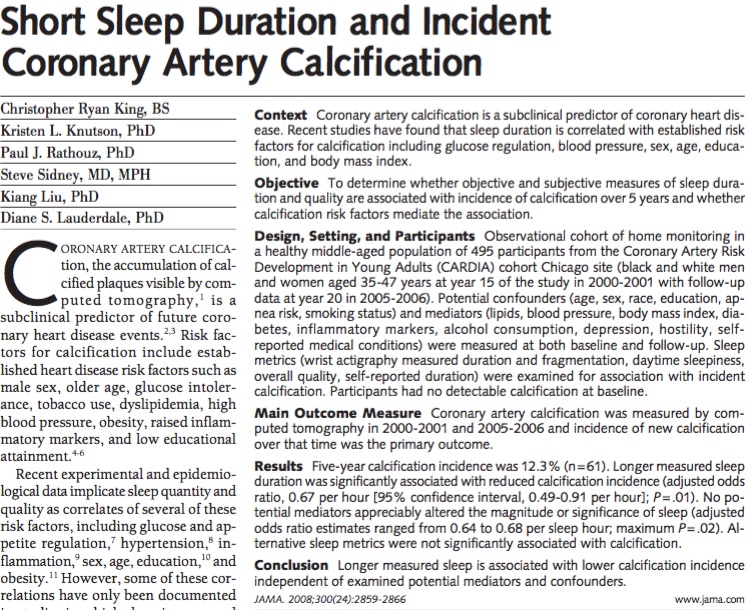
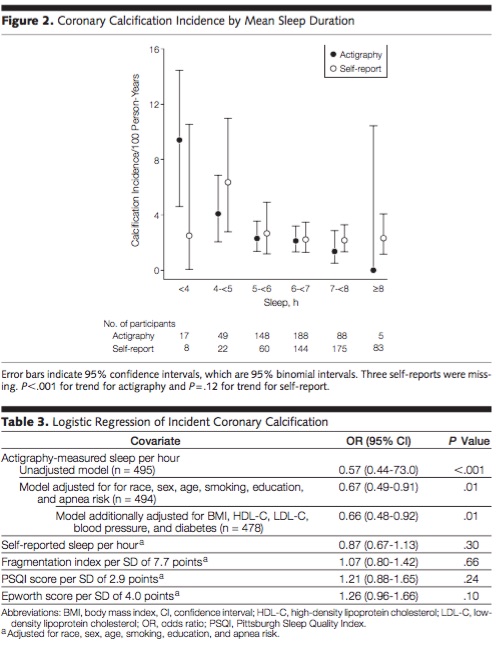
Sleep saves lives
Interesting article looking at nightly sleep and coronary calcification. Pretty scary. Here is the abstract and a notable chart. They used actigraphy (wrist devices) to measure sleep and found a big difference, as many trials have, between self reported sleep and measured sleep. Sleep one extra hour a night and drop your coronary calcium by 33% (obviously this is a statistical finding and not an intervention study, still striking).
Hypertonic Saline vs Mannitol
Research and Reviews in the Fast Lane (which is a must for anyone consuming FOAM) just covered a SR and meta-analysis on hypertonic saline. Relevant after our discussion in conference this morning.
Berger-Pelleiter E, et al. Hypertonic saline in severe traumatic brain injury: a systematic review and meta-analysis of randomized controlled trials. CJEM 2016. PMID: 26988719
- Hypertonic saline seems to be recommended more and more often for intracranial hypertension. What is the evidence in traumatic brain injury?
This is a systematic review and meta-analysis that identified 11 RCTs covering 1820 adult patients with traumatic brain injury comparing hypertonic saline to either mannitol (½ the studies) or another solution (often normal saline, or even hypotonic saline.) Hypertonic saline did not decrease mortality (RR 0.96, 95%CI 0.83-1.11). It didn’t lower intracranial pressure (weighted mean difference -0.39, 95%CI -3.78 – 2.99). And it didn’t improve functional outcomes (RR 1.12, 95% CI 0.92-1.36). Maybe we shouldn’t be rushing to adopt hypertonic saline in the management of traumatic brain injury.
- Recommended by Justin Morgenstern
Journal Club July 2016
Just say NO to DESAT
I was about to spend a lot of time on a post here about pre oxygenation, specifically re: apnea oxygenation with nasal cannula. I was inspired be yet another favorable article in this month’s Academic EM (which by the way is going to be online ONLY as of Jan 2017).
Then realized Weingart had of course already posted a ridiculously good synopsis of what was out at the time.
If you plan at anytime in the future to intubate a human patient, STOP what you are doing and read the Emcrit post before your next intubation.
Add to his post the new article. And the common sense that a nasal cannula has no risk to the patient. There is just no reason not to place a 10L or greater nasal cannula on all patients during intubation.
Just finished writing the post and noticed EMLitofNote just reviewed this article, also linked to a LITFL post and a Rebel EM post. Their conclusions are similar, though they call for an RCT. Not sure we need to spend a bunch of money on an RCT. I say just use the cannula for 5 minutes while you intubate.
New Residents
This advice applies to all residents and most of it works for physicians of all ages.
Sick PEs
We had a very ill patient recently. She was found down upstairs visiting her family member. She was calmly altered, not agitated but was in mild distress. Consciousness fluctuated. Tachycardic and hypertensive initially, then had more labile BP and some hypotension.
We had to intubate her due to poor MS and clinical condition. She coded in CT, we placed a central line on the CT table between her noncontrast head CT and her CT chest. We pushed an amp of Epi and ran out of the room for the CT chest. We were worried about dissection and PE in equal amounts. We could not get good cardiac windows on bedside Echo in room 9 prior to the CT.
She continued to intermittently lose her pulse and drop her BP. We confirmed bilat PEs on the CT when we saw NO contrast left her right ventricle. The CT tech noticed first and became worried the patient had no cardiac output (ie pulseless).
We rushed the patient back to room 9 and gave a tPA bolus (50mg) followed by infusion of 40mg. She was on pressors and heparin and improving. Dr Smith accepted her to Jewish for possible EKOS or even ECMO if needed. On arrival to Jewish a few hours later she coded and died.
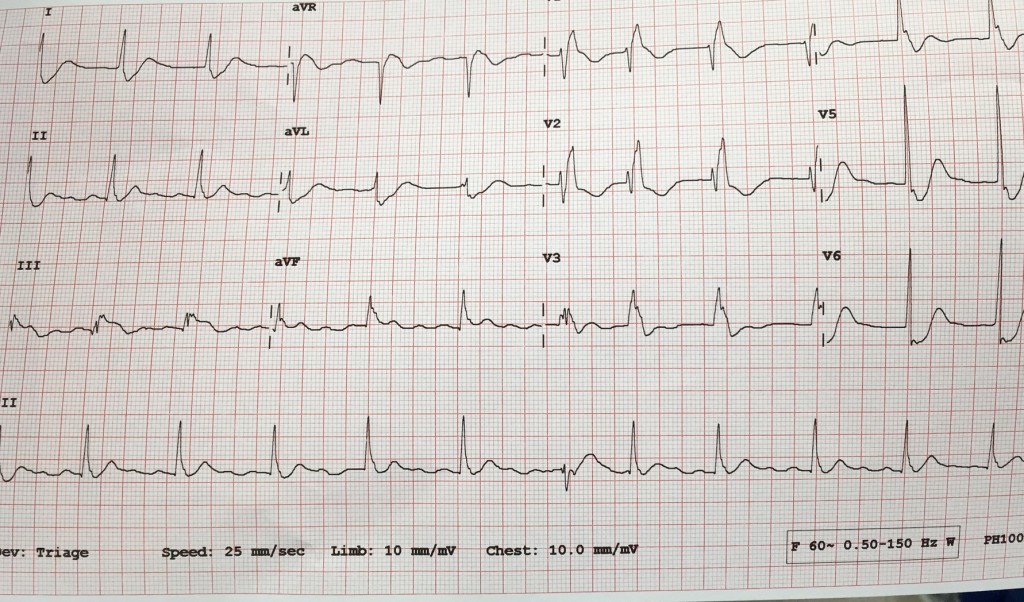
I was surprised when I found out she had died. Her O2 sat was improving, HR was decreasing, blood pressure was stable (though dependent on pressors). She received a large amount of crystalloid IV which according to some data might not have been optimal management. She also had the following ECG:
I think she was infarcting her myocardium. She likely had pulmonary infarction considering her poor oxygenation. She had coded a few times. She had a lot of strikes against her. Her BEST SHOT was going to a place with catheter assisted treatment for PE and ECMO if needed.
I am posting the case to let everyone know:
- How to manage sick PE patients (see post below)
- To use tPA in massive and in many cases of submassive PE
- TRANSFER sick PE patients to Jewish for EKOS/ECMO
- The decision to diagnose PE with RV strain on BEDSIDE Echo with no formal Radiologic testing will depend on your attending
This post from EmCrit / PulmCrit is a beautiful summary with potential dogmalysis related to PE management (see take home points below but do read the post).
In addition, here is a nice review article on catheter-based reperfusion treatment for PE with nice references for further reading.
Take home points from the Emcrit post:
- The only evidence-based intervention that seems to improve mortality in massive PE is thrombolysis. The primary goal of therapy should be administration of thrombolysis as soon as possible to patients without contraindication.
- Consider early stabilization of blood pressure using a norepinephrine infusion, administered peripherally if necessary.
- Volume administration may facilitate dilation of the right ventricle and hemodynamic deterioration.
- Intubation is very hazardous and should be avoided if possible. Patients die from cardiovascular collapse, and intubation may worsen this.
- For a coding PE patient consider 50mg alteplase bolus as well as an infusion of epinephrine. Patients can do well despite requiring CPR and high dose vasopressor infusions.
Drug Interactions
Not sure if anyone follows David Juurlink on Twitter. He posts a lot on the opioid epidemic amongst other pharm and to topics. Here is a lecture on dangerous drug interactions. You can watch the video or skim the slides.
Head injury patients with delayed presentation to ED
Another pearl from EM Lit of Note. Bottom line: Retro review of CT head obtained for trauma divided into <24 hours and >24 hours time of presentation. The delayed presenters had a HIGHER percentage of positive CT and had a similar amount of patients requiring NES intervention.
We discussed this the other day. First Care obtained a head CT on a patient several days after a minor head injury. We presumed it was not indicated. Then I read this paper.
Unfortunately I cannot find in the paper a description of time to presentation. It is grouped into less than 24 hours and greater than. I wonder if the likelihood of positive CT scan decreases as time from injury to presentation increases.
In any event, this poses difficult questions. Should we obtain more CTs on the delayed presenters? They are as likely to have positive findings. In addition, the NICE guideline is 70% sensitive, versus its comforting 98% in the less than 24 hour group.
Would be a good article to discuss for journal club. Would love to see some comments.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)