Apparently I’m a magnet for ocular trauma. Oddly enough, it’s the one thing that still makes me queasy. Anyways, I feel like over the past year I’ve dealt with quite a few cases of orbital compartment syndrome, mostly which have been traumatic in nature. After having done a few lateral canthotomies, I have a few pearls that may help others along the way. I think the hardest part of the entire procedure is making the decision to actually do it.
You should have suspicion with any patient presenting to the ED with any obvious facial trauma. I generally start off with gross testing of visual acuity, seeing if patient can see first light, then the number of fingers that I’m holding up. If they can see both, then my suspicion is much lower. What generally makes me more concerned is when the patient states they cannot see out of one eye. Often, in the case of trauma, this will be secondary to significant swelling causing the lids to be swollen shut, which obstructs the patient from physically opening their eye. If you manually open it, the hope is that they will be able to see.
This is where things can get muddy. Most often, when their lids are this swollen, you’re going to have a difficult time manually opening the lids. Also, if it’s traumatic related, theres likely to be blood around the eye which adds in another layer of difficulty of opening the eye. Optho has some really nice ocular forceps, but I don’t believe we have them in our canthotomy tray.
The easiest way that I have found to open both lids is with the use of two paperclips. First I wipe them off with alcohol and then bend them in such a manner that one of the curved ends is folded backwards. This will allow you to have a smooth, rounded object to elevate the eye lid. Obviously, DO NOT DO THIS IF YOU ARE CONCERNED FOR AN OPEN GLOBE.
I feel like in most of these patients, they have significant chemosis noted to the sclera which looks like the photo below. Seeing this also makes me concerned that theres a reason the sclera is so congested (vascular congestion secondary to obstruction).

Once you have the lid retracted, now is time to establish if the patient has vision in that eye. You’re going to want a helper to keep the lids retracted. I attempt to get the patient to see how many fingers I’m holding up. If they can’t see that, I try and figure out if they can see light. If the patient states that they cannot see, I “challenge” their vision in that eye, most often by flicking a finger close to their eye in a rapid manner to see if they blink. A normal person is not going to let you flick at their eye without blinking. If they don’t blink, I start to get more concerned.
The next piece of info you’re going to want is to get a pressure. It seems like majority of the ones I have done, pressures have been in the upper 40s to 50 or either the tonopen reads “err.” Keep in mind if you use the tonopen too aggressively, you will get a falsely elevated pressure.
If I have gotten this far and I’m still convinced that the patient has no vision in the eye and their ocular pressures are elevated, I’m getting set up to perform the canthotomy. I’m of the notion that if it’s THAT important to do emergently, I’m going to call opthamoloy after I have treated the emergency.
Ideally, the procedure is best done in room 9 if you are capable for a few reasons
#1: the overhead lights in there are great and vastly improve your visibility during the procedure.
#2: you’re going to want to sedate the patient to make it more comfortable. I typically use fent/versed. i try to avoid ketamine for the theoretical idea that it likely increases IOP.
#3: the lateral canthotomy tray is in bay 4. if you’re standing at the foot of the bed, its immediately on your right, like the 2nd shelf from the top in the pixis closest to you.
So you’ve decided to do the canthotomy. Lighting is great. You have your tools at bedside. You’ve got the patient hooked up to the monitor. You’re all ready to sedate the patient. You push drugs and start the procedure. At this point, you’re going to want to start anesthetizing the region. To do this, start AT the lateral canthus and orient your needle AWAY from the globe. You want to inject out towards the lateral orbital rim, away from the eye ball. While you’re injecting, this is giving your patient time to start having some effects of the sedation.
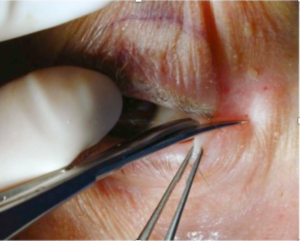
After you have anesthetized the area, take a few saline flushes and rinse out the eye in case there is in foreign debris. Next, in theory you should use a hemostat to “crimp” the margin at the lateral canthus. Optho has rolled their eyes at me when I’ve done this and they say it isn’t necessary. The idea is that it is supposed to help it not bleed as bad when you cut this area. I personally don’t do it for the hemostatic purposes. I feel like crimping the area generally helps get a small amount of swelling out of the way so I can fit in the tips of my iris scissors when I go to make the first cut. This is ultimately why I continue to do this part of the procedure.
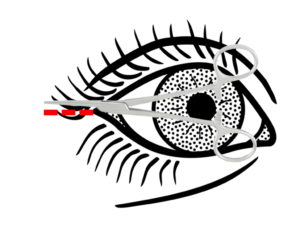
After you have crimped the tissue for 10-20 seconds, remove the hemostats. You’re going to want to use the iris scissors at this point in time. You’re going to encounter some difficulty because both lids are edematous and likely there is significant edema in the sclera. You’re going to be shitting yourself because it’s hard to tell what’s sclera and what is skin/skin structure. This is when the overhead lights in room 9 REALLY help make a difference. Once you are able to identify the lateral canthus, open the iris scissors and insert one blade below the lateral canthus directed away from the eye. You are going to want to bluntly disect infero-laterally towards the lateral orbital rim. Your ultimate goal will be to cut ~1cm of the skin overlying the lateral canthus and then disect down to the lateral canthal tendon, just medial to Whitnall’s tubercle.
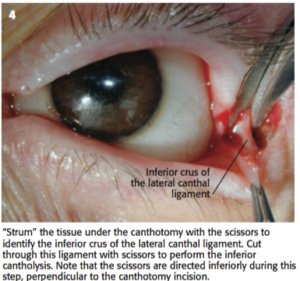
At the lateral canthal tendon, there will be two bands of fibrous tissue; the superior and inferior crus. Generally it is the inferior crus that is relieved first in this procedure.
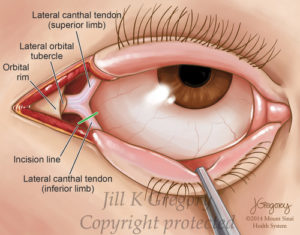
At this point, things are going to be a bloody mess, so the best way to identify them is to use the tip of your iris scissors and literally “strum” the tendon. It will feel exactly how you expect it to feel. You will feel the tendon strum. When you do this, make small movements, almost like micro-movements. As you strum the crux, you will be able to tell where one side starts and terminates. You may be able to physically see it if you’ve disected well enough. Regardless, you can use the tips of the iris scissors to envelop the crux and make the cut. If you have done this correctly, you should appreciate that the lid has relaxed. If the eyelid doesn’t feel any more mobile than previous, take a deep breath. Try and use some 4x4s to clear away the blood and take a better look. Likely you haven’t fully transected the ligament if the lid isn’t relaxed, even if you think that you might have.
If you have been successful, you will be able to appreciate that the lid is less constrictive of the globe. Now, go ahead and check your pressures at this point. Assuming that the pressures are significantly improved, you’re done. Say your pressure wasn’t reading prior to the procedure and now its still in the upper 40s and you have verified that you have transected the inferior crus, the patient will likely need the superior crus transected as well. You are capable of doing this; however, if you’re uncomfortable, optho will likely do it when they arrive. Just go about transecting the superior crus in the same fashion.
Speaking of optho, now that the emergent situation has been handled, this is the time to give them a call and let them know that you’ve decompressed the patient’s orbit. They will come in and do their thing and you can carve another notch in your belt.
_____________________________________________________________________________
On a side note, I had a non-traumatic orbital compartment syndrome a few months back. The guy came as a transfer from an outside facility with unilateral vision loss, proptosis, and headache. CT at OSH showed an intraorbital mass. I’m not certain why, but given it was not traumatic, I didn’t think to immediately decompress his orbit as his symptoms had been persistent over the past two days and not acute in onset. Make note, it is still completely acceptable and recommended to perform a canthotomy in this setting. Just something that I realized in hind-sight.

Anyways, this is a lot of reading. If you made it to here, thanks. Hopefully this was somewhat clear. If you have any questions, I’m happy to answer.
References:
Roberts and Hedges Clinical Procedures in Emergency Medicine – Opthalmologic Procedures: Chapter 62 pg 1295.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)