- Termination of resuscitation (Nichols)
- When to stop resuscitation in out of hospital arrest
- DNR order
- No chance of saving them–safety, signs of irreversible death
- Nothing left to do–unwitnessed arrest, no shockable rhythm, ROSC does not return in the out of hospital setting
- Stop CPR if:
- No ROSC
- No shocks
- Unwitnessed
- When to stop resuscitation in out of hospital arrest
- CCU follow up (French)
- Arrhythmogenic RV dysplasia
- 2nd MCC sudden cardiac death in young patients
- Greek or Italian descent
- Male:Female= 3:1
- Presentation
- Asymptomatic
- Palpitations
- Syncope
- Ventricular dysrhythmias/cardiac arrest
- FH of unexplained syncope/sudden death
- RV failure
- Cards consult–>admission
- Arrhythmogenic RV dysplasia EKG: V1-V3 T wave inversions, epsilon wave
- HOCM EKG changes: high voltage, LVH, lAD, tall R wave V1
- Arrhythmogenic RV dysplasia
- MICU follow up (Schutzman)
- Myxedema coma
- Hypotension
- Bradycardia
- Electrolyte derangements
- Altered mental status
- Give levothyroxine
- Myxedema coma
- Jeopardy (Daughtery)
- Activated Charcoal
- Adsorbs toxins and inhibits GI absorption
- Must be given in 1-2 hours, but still consider if ingested drug is extended release
- Contraindications: GI perforation, need for endoscopic procedures
- Concerns: emesis, CNS depression and aspiration risks
- Consider risk vs benefit of administration
- Deferoxamine
- MOA: complexes with trivalent ions (ferric ions) to form ferrioxamine which is eliminated in urine by the kidneys
- Indications: iron level >500, metabolic acidosis, lethargy/coma, shock, toxic appearance
- Can cause urticaria, flushing of skin, hypotension, shock with rapid IV administration, ARDS
- Itralipids (lipid emulsion)
- Reversal of local anesthetic systemic toxicity
- Consider for severe hemodynamic compromise of lipophilic xenobiotics or drugs with significant neurological or CV toxicity–last line
- 20% emulsion solution
- Phentolamine
- MOA: competitively blocking alpha adrenergic receptors
- Indicated in pheochromocytoma hypertensive crisis, extravasation of norepinephrine/epinephrine, hypertensive emergency with end organ damage secondary to cocaine toxicity not responsive to appropriate sedation
- Concerns: hypotension, medication safety
- Levocarnitine
- Antidote to valproic acid
- Give when: moderate to severe hyperammonemia, valproate level >450, CNS depression, severe hepatotoxicity
- Naloxone for clonidine reversal
- Big doses- 10mg
- Consider for reversal of CNS depression
- Fluids and vasopressors may also be required
- Benzodiazepines
- Midazolam: IV onset of action 2 min
- Lorazepam: onset of action 5-20 minutes
- Physostigmine
- Reversal of anticholinergic toxicity
- Primarily for agitation and delirium reversal
- MOA: inhibits acetylcholinesterase and prolongs the central and peripheral effects of acetylcholine
- Have physician and atropine at bedside
- No significant risk of seizures
- Low dose, push slow
- Flumazenil
- Benzodiazepine overdose or reversal only
- Competitively inhibits activity of BZ receptor site on GABA/BZ receptor complex
- Not effective on other medications that affect GABA
- Concerns
- Could precipitate withdrawal seizures if patient regularly uses benzos
- Seizure history outside of withdrawal seizures
- Risk vs benefit–goal of therapy
- Activated Charcoal
- Project ECHO
- Optimal Aging Clinic will be added to discharge follow up options
- Have a “what matters” conversation
- Advance Directives
- Living will
- POA
- POLST/MOST
- EMS DNR
- Advanced care planning–ICD code, must spend 16 minutes to bill
- MOST form
- A physician’s order
- Must be honored by all KY healthcare providers in all KY settings
- State of KY Hierarchy of Decision making authority if no advance directives
- Court appointed guardian
- Healthcare surrogate
- Spouse
- Adult children
- Parents
- Adult siblings
- Closest living relative
- ECMO (Ritchie)
- Components
- Motor/pump
- Filter/oxygenator
- Blender
- Ventilation–to increase, go up on gas flow aka sweep
- Oxygenation–to increase, go up on blood flow aka flow
- Cannulas (single vs double)
- Circuits
- Vein-Vein ECMO
- Is the heart still able to pump
- Vein-Artery ECMO
- Heart pump function not ideal
- Vein-Artery-Vein ECMO
- Vein-Vein ECMO
- VV ECMO
- Indications
- Hypoxic respiratory failure, 50% mortality risk consider ECMO
- Hypoxic respiratory failure, 80% mortality risk, put on ECMO
- CO2 retention on mechanical ventilation despite high Pplat
- Severe air leak syndromes
- Need for intubation in a patient on lung transplant list
- Immediate cardiac or respiratory collapse (PE, blocked airway, unresponsive to optimal care)
- Anytime patient is on dangerous vent settings
- Murray Score: conventional ventilation or ECMO for severe adult respiratory failure
- Score of 3–consider transfer to ECMO center
- Score of 4– ECMO indicated
- Contraindications
- No absolute contraindications
- Mechanical ventilation at high settings for 7 days or more
- Major pharmacologic immunosuppression
- CNS hemorrhage that is recent or expanding
- Non-recoverable co-morbidity
- No absolute contraindications
- When making the decision to begin ECMO
- Is this condition reversible?
- Is it a bridge to transplant?
- RESP score (estimated survival once on VV ECMO)
- ARDS
- Ventilator trauma
- Volutrauma
- Barotrauma
- Atelectrauma
- Biotrauma (cytokine storm, inflammation)
- Energytrauma (goal for driving pressure 15 or less)
- Settings once cannulation successful
- Set flow: 4L
- Set Sweep: 4L
- Lung rest settings while on ECMO
- PC 10/10/10/40%
- Goals
- Sat >85%
- MvO2 >65%
- Indications
- VA ECMO
- Indications
- Heart failure bridge to recovery, heart transplantation, VAD
- Cardiogenic shock
- Myocarditis
- ECPR
- Right heart failure
- PE
- Medication overdose
- SAVE score
- Indications
- Trans pulmonary pressure
- Consider in morbidly obese patients
- May have higher PEEP requirements given pressure from chest wall/abdomen
- When intubated, they lose the ability to autopeep
- Page Jewish thoracic or cardiac surgery –consult early
- Components
Author Archives: ccapocaccia
Conference Notes 1/13
- ITE- grab bag (E Thomas)
- Spider bite, necrotic wound>brown recluse
- MCC erythema multiforme> HSV
- Strawberry cervix>trich
- Pre-E, less than 24 weeks>mole pregnancy
- Abdominal pain after sex>ovarian torsion
- Most common personality disorder>borderline
- Patient intentionally fakes symptoms>malingering
- Sudden paralysis after traumatic event>conversion
- Discriminatory zone for TVUS>1500
- PID/RUQ pain/shoulder pain>Fitz Hugh Curtis
- MCC postpartum hemorrhage>uterine atony
- Pizza pie fundus>CMV
- Corneal dendrites>HSV keratitis
- Tachycardia out of proportion to fever>thyroid storm
- Alcohol, AMS, ataxia, nystagmus>wernicke
- Stingray wound>hot water
- Beta blocker OD>hypoglycemia
- One Pill Can Kill (Lund)
- Ingestions–fatal in small doses
- CCB
- Cyclic antidepressants
- Lomotil
- Opiates
- Salicylates
- Toxic alcohols
- Sulfonylureas
- Camphor
- Clonidine
- Antimalarials
- CCB OD
- Hypotension, bradycardia, bradydysrhythmias, hyperglycemia
- Tx: charcoal, fluids, atropine, calcium, intralipid
- Salicylates
- Oil of wintergreen, ASA, pepto-bismol
- n/v, tinnitus, delirium, hallucinations, pulmonary edema, cerebral edema, mixed anion gap metabolic acidosis with respiratory alkalosis
- Sulfonylureas
- Hypoglycemia, lethargy, irritability, confusion, HA, seizures
- Tx: observation x24 hrs
- Dextrose bolus, then consider infusion
- Can give octreotide (inhibits secretion of insulin)
- Clonidine
- Alpha 2 agonist, (afrin, visine)
- Opioid syndrome: lethargy, coma, miosis, respiratory depression
- Tx: naloxone, atropine, IV fluids, inotropes
- Camphor
- Campho-phenique, vicks vaporub
- GI distress, generalized warmth, CNS hyperactivity, CNS depression, n/v, oropharyngeal irritation/burning/stinging
- Tx: benzos, phenobarb
- Amitriptyline
- CNS depression, seizures, cardiac conduction abnormalities (QRS prolongation), hypotension, mydriasis, flushing, dry mucous membranes, hallucinations, hyperthermia
- Tx: benzos for seizures, sodium bicarb for QRS widening >100ms
- Lomotil
- Opioid receptor agonist +/-atropine
- Classically biphasic, with anticholinergic symptoms 2-3 hours s/p ingestion followed by opioid symptoms
- Tx: naloxone
- Dispo: admit
- Ingestions–fatal in small doses
- Toxic Alcohols (Bosse)
- Ethanol
- Can cause hypoglycemia
- Is dialyzable
- Isopropanol
- Rubbing alcohol
- Metabolized to acetones
- No metabolic acidosis
- Supportive treatment, can be dialyzed
- Methanol
- Windshield washer fluids, solid cooking fuel, embaling fluid, tainted beverages
- Toxic metabolite is formate (formic acid)
- CNS effects, visual effects, pancreatitis, symptoms delayed in onset
- Metabolic acidosis with elevated anion gap
- Ethylene glycol
- Antifreeze (sweet taste)
- Toxic metabolites: oxalate, glycolaldehyde, glycolic acid, glyoxylic acid
- CNS effects, metabolic acidosis, renal toxicity, myocardial dysfunction
- Oxalate can cause hypocalcemia by calcium oxalate precipitation
- Oxalate crystals in urine
- Wood’s lamp to urine, antifreeze products may contain fluorescein, not a great test
- Osmol gap
- Difference between measured serum osmolality and calculated serum osmolarity
- Normal serum osmolality: 275-295 mOsm/kg
- Antidotes
- Ethanol, fomepizole
- Competitive inhibitors of alcohol dehydrogenase
- If ethanol must be used, give orally. Keep blood level >100mg/dL
- Treat if methanol or ethylene glycol level >20mg/dL
- Can be stopped once level less than 20mg/dL
- Dialysis
- Consider if patient has end organ manifestations (even if levels undetectable)
- Folic acid for methanol
- Thiamine and pyridoxine for ethylene glycol
- Send methanol and ethylene glycol levels ASAP
- Ethanol
Conference Notes 1/6
- Aspirin Toxicity (Harmon)
- Sources of salicylates
- Aspirin
- Oil of Wintergreen
- Pepto-Bismol
- Bengay
- Alka-Seltzer
- Skincare products
- Mechanism of toxicity
- Fatal dose 10-30 g in adults
- Dose dependent
- Acute vs chronic
- Increases respiratory center sensitivity, uncouples oxidative phosphorylation, inhibits TCA cycle/amino acid metabolism, stimulates chemoreceptor/trigger zone
- signs/symptoms
- Tinnitus, nausea, vomiting, dizziness, fever
- Ataxia, anxiety, lethargy, AMS, seizure, arrhythmias, seizure
- Evaluation in ED
- Serum salicylate concentration and trend
- ABG
- CBC, CMP, coags, EKG, UA, tox
- Management
- Gastric decontamination (ingestion w/in past 1-2 hours)
- Sodium bicarb (consider if level >40)
- Avoid intubation as long as possible
- Fluids
- HD
- Poison Control
- Sources of salicylates
- Acetaminophen Toxicity (Cook)
- Signs/Symptoms
- Stage I: anorexia, n/v, elevated transaminases
- Stage II: RUQ pain, elevated transaminases
- Stage III: hepatic failure, acidosis, renal failure, pancreatitis, peak transaminase levels
- Stage IV: multi-organ failure vs resolution
- Lab Assessment
- APAP levels
- Within 1-4 hrs of ingestion, used to exclude ingestion
- Obtain 4 hour level to get estimated peak absorption
- CBC, CMP, ABG
- APAP levels
- Rumack Matthew Nomogram
- Treatment line
- begins at 4 hr mark
- If above line, treat
- Treatment line
- Treatment
- Activated charcoal
- N-Acetyl Cysteine
- Replenishes glutathione stores to conjugate NAPQI to limit hepatocyte injury and promote renal excretion
- Signs/Symptoms
- TCAs (Weeman)
- MOA
- SSRI/SNRI, antihistamine, alpha antagonist, anti-muscarinic
- Symptoms
- Early: anticholinergic effects, HTN, AMS
- Late: myocardial suppression, QRS widening, seizures, ventricular dysrhythmia, hypotension
- Mimics: diphenhydramine, carbamazepine, sympathomimetic toxicity, serotonin syndrome
- Assessment
- EKG, UDS, TCA level (does not correlate with severity)
- Management
- Activated charcoal if within 1 hour of ingestion
- Do not treat early HTN as patients will likely develop hypotension as they progress, treat hypotension with normal saline
- Sodium bicarbonate
- IV push if QRS exceeds 100 msec
- Infusion to maintain pH 7.5-7.55
- If seizing, use IV benzos or phenobarbital if refractory
- MOA
- Clinical Pathway Opioid Overdose (Leavitt, Sizemore)
- Duration:
- Heroin half life: 3-8 min, metabolites ~3hrs
- Fentanyl half life: 2-4 hrs
- Oral opioid half life: 3 or more hours
- Narcan
- Opioid antagonist
- In general, don’t exceed ~5-10 mg, but can titrate to effect
- Route
- IN/IM/SC: slower onset, longer duration
- Intranasal can last ~3hrs
- IV
- Infusion:
- Mix 4mg naloxone in 100 mL D5W
- Infusion rate at ⅔ of effective dose that initially reversed the patient
- Can repeat dosing every 3 minutes
- St. Paul’s Early Discharge Rule
- HOUR Study
- Clinical Pathway to be posted soon
- Duration:
- Envenomation (Giddings)
- Ciguatera
- Heat stable toxin
- Barracuda, red snapper, mostly reef/tropical fish
- GI symptoms, paresthesias, hot/cold reversal, bradycardia
- Treatment: antiemetics, atropine, mannitol
- Mechanism: increases permeability of sodium channels inducing membrane depolarization
- Scombroid
- Caused by improperly stored fish, heat stable toxin
- Symptoms: flushing, warmth, urticarial rash, palpitations, itching
- Causes histamine release
- Tx: antihistamine
- Coral Snake (Elapidae)
- Presentation: minimal local symptoms, severe systemic symptoms, respiratory paralysis, AMS, CN palsies
- Complications: hypovolemic shock, DIC
- Work up: CBC, CMP, coags, fibrinogen, d-dimer
- Treatment: anti-venom, aggressive supportive care
- Dispo: Admit, concern for neurotoxic effects including respiratory failure, can have delayed presentation
- Mechanism: cholinergic
- Crotaline (Pit Vipers)
- Presentation: Local pain/tissue damage, fang marks, coagulopathy, weakness, n/v
- Complications: swelling, compartment syndrome, DIC, hypotension
- Treatment: CroFab (give if bad systemic symptoms, abnormal labs, AMS, significant swelling)
- Black Widow
- Presentation: Pinprick bite, pain to whole extremity, muscle cramps, tachycardia, hypertensive, can mimic appendicitis
- Management: supportive care, antivenin for severe symptoms
- Tarantula
- Barbed hair, can penetrate cornea, may need ophthalmology consult
- Supportive care
- Brown Recluse
- Painless bite, local tissue necrosis
- Systemic effects are rare
- Treatment: supportive
- Ciguatera
- High Altitude Medicine (Thurman)
- Physiology
- High Altitude: 1500m, Very High: 3500m, Extreme: 5500m
- Begin to see altitude illness at around 2500m/8000ft
- As altitude increases, percentage of oxygen available decreases
- Acclimatization
- Respiratory compensation by increasing minute ventilation, which decreases PaCO2
- Renal compensation by increasing excretion of bicarbonate
- Associated diuresis can exacerbate altitude illness and increase dehydration
- Acute Mountain Sickness
- Headache, GI symptoms, fatigue/weakness, dizziness/light-headedness
- Prevention (ideally start 1 day before trip, continue 1-2 days after patient is at highest altitude)
- Acetazolamide 125 mg q12hr
- Dexamethasone 2mg q6hr or 4mg q12hr
- Gradual ascent
- Ibuprofen 600 mg q8hr
- Treatment
- Halt ascent until symptom free
- Only need to descend for severe symptoms
- Supplemental oxygen, dexamethasone, acetazolamide
- High Altitude Cerebral Edema
- Acute mountain sickness + mental status change, ataxia
- Treatment
- Immediate descent/evacuation
- Supplemental oxygen
- Dexamethasone
- Portable hyperbaric chamber
- Acetazolamide
- High Altitude Pulmonary Edema
- Non-cardiogenic pulmonary edema
- Symptoms (need at least 2)
- Dyspnea at rest
- Cough
- Chest tightness/congestion
- Weakness/decreased exercise tolerance
- Signs (need at least 2)
- Crackles or wheeze
- Central cyanosis
- Tachypnea
- Tachycardia
- Prevention
- Gradual ascent
- Nifedipine 30 mg q12hr or 20 mg q8hr
- Tadalafil/Sildenafil
- Treatment:
- Immediate descent
- Supplemental oxygen
- Nifedipine
- Portable hyperbaric chamber
- tadalafil/sildenafil
- CPAP
- Physiology
- COVID (Brown)
- Symptoms
- Typical of most viral syndromes
- Lab abnormalities
- Elevated WBC, LDH, d dimer, ferritin, ESR/CRP, procal, ALT/AST, t bili, troponin, CK
- Low lymphocyte count, albumin, platelet count, hemoglobin
- Imaging
- Normal vs bilateral pulmonary opacities
- Airway management
- Pre-oxygenate with NRB or HFNC
- Consider supraglottic airway with viral filter
- Video laryngoscopy
- Trial HFNC or non-invasive ventilation prior to taking airway
- Low tidal volumes, permissive hypercapnia, ARDSNet protocol
- Consider proning
- Treatment
- Supportive treatment
- Bamlanibimab
- Dexamethasone
- Remdesivir
- DVT ppx if hospitalized
- Disposition
- Walking O2 test
- 4C mortality score
- Symptoms
- Pacemakers (D. Thomas)
- Prevent HR from falling below set limit
- Pacing
- Sensing
- Malfunction
- Failure to capture
- Low battery
- Inflammation
- Loose or displaced lead
- Sensing issues
- Undersensing
- Oversensing
- Failure to capture
- Management
- Typical bradycardia management
- Atropine, epinephrine, transcutaneous pacing, transvenous pacing
- Magnet placement
- Opens Reed switch with breaches sensing circuit and will pace regardless of intrinsic cardiac activity
- Prevent HR from falling below set limit
Transvenous Pacing
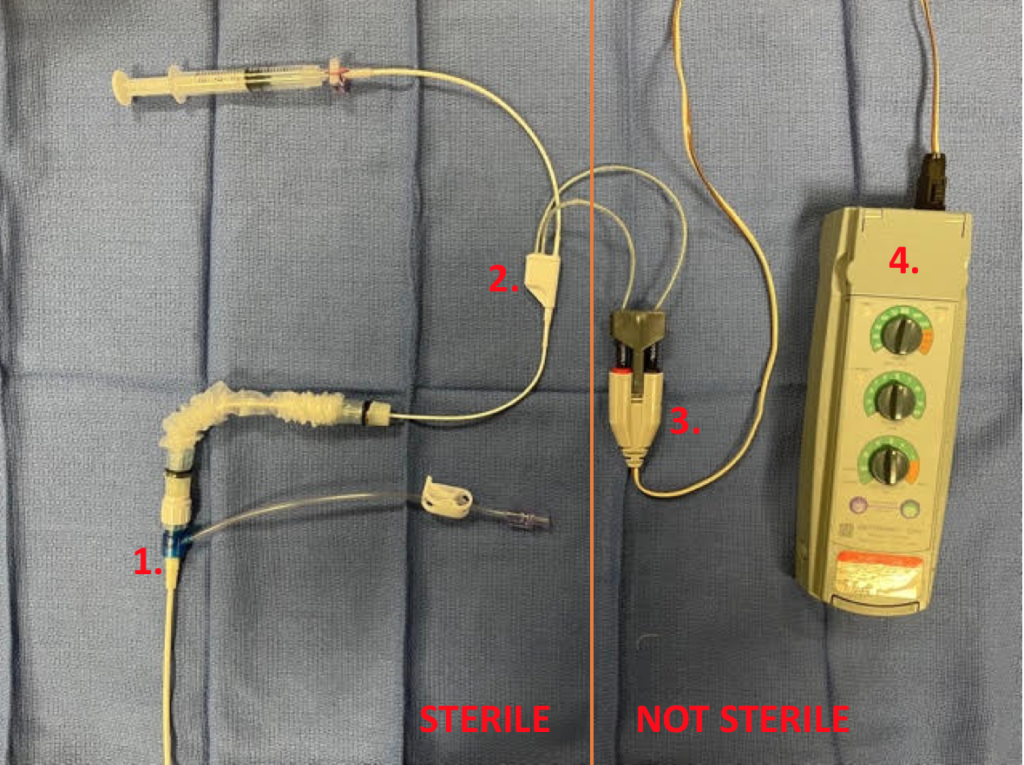
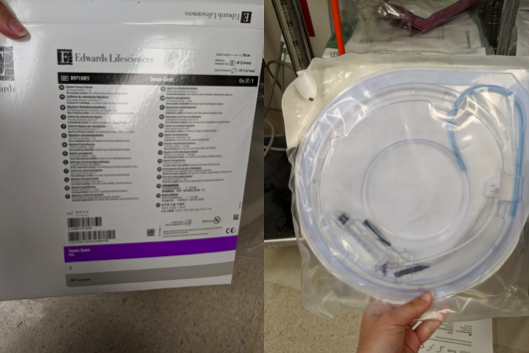
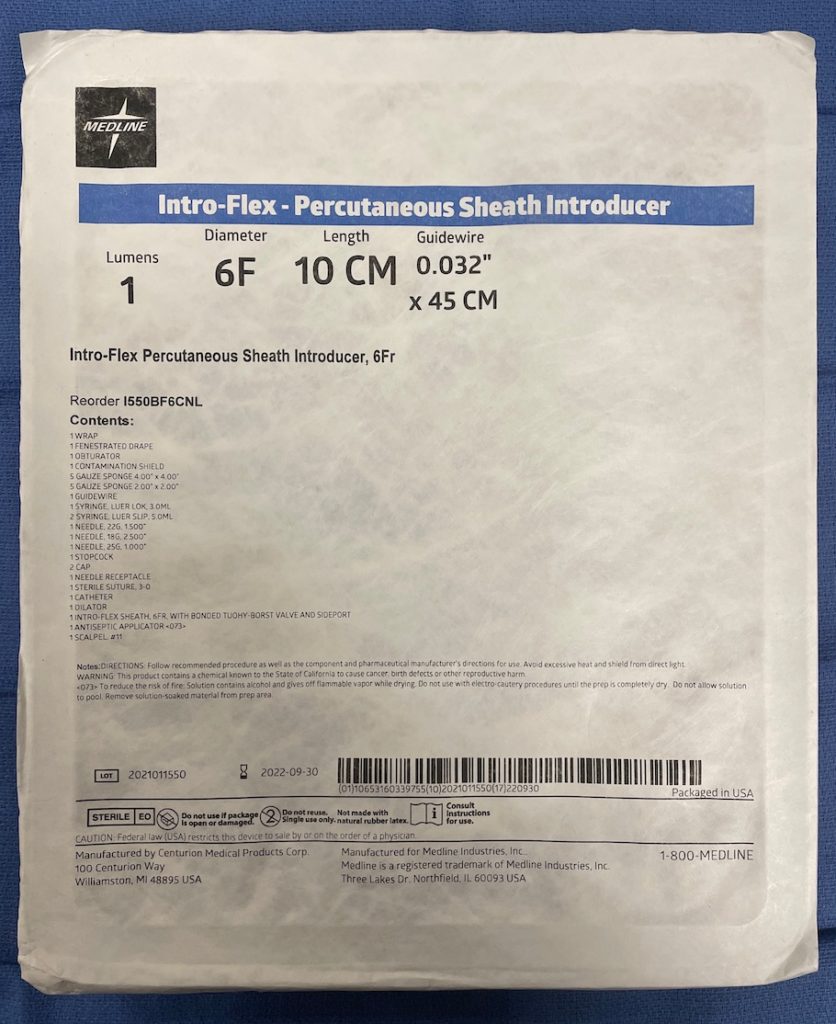
1. 6F Cordis
2. Swan Ganz Pacing Catheter
3. Nonsterile Connecting Cable
4. Pacing Generator
Indications
- Symptomatic sinus bradycardia (after atropine, +/- dopamine/epinephrine, and transcutaneous pacing have failed)
- Mobitz type II second degree AV block
- Complete heart block
- Beta blocker or calcium channel blocker overdose
Preparation
- Patient positioning: supine/Trendelenburg
- 6 French Cordis (“percutaneous sheath introducer kit”)
- Swan Ganz/Bipolar pacing catheter
- Pacer generator (“temporary pacemaker”)
- Nonsterile connecting cable (within pacer generator case in inside sleeve)
- Ultrasound + sterile probe cover
Supplies and room 9 location

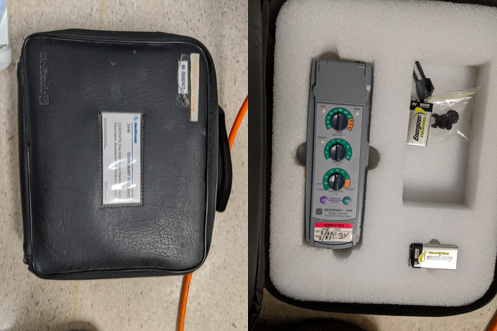
Pacer generator—initial settings
- Turn on
- Rate—80 bpm, rate at which patient will be transvenously paced, at least 20 bpm over the intrinsic rate
- Output—20 mA, electrical output of pacer with every paced beat, decrease until patient has both mechanical (palpating patient’s pulse) and electrical capture
- Sensitivity—3 mV, pacer’s ability to sense intrinsic rate (the lower the sensitivity, the more the pacer will detect intrinsic rate; for example, at 3 mV, the pacer will only detect impulses generated from the heart that are greater than 3 mV)
- Oversensing- Sensitivity is set too LOW so electrical signals are inappropriately recognized as cardiac activity and pacing is inhibited
- Undersensing- Sensitivity is set too HIGH so pacemaker ignores native cardiac activity
Location
- Right internal jugular—preferred
- Left subclavian—use as second option, preferred to leave site available for possible permanent pacer
Steps to placing transvenous pacemaker
- Place cordis
- Set up nonsterile connecting cable (helpful to have assistant connect cable to pacer generator as these are not sterile)
- Ensure proper balloon inflation on Swan Ganz
- Position sterile sleeve over pacer wire and ensure correct orientation
- Insert pacer wire into cords and advance to 20cm (indicated by first two black lines)
- Insert Swan-Ganz + and – pins into nonsterile connecting cable (proximal to positive, distal to negative)
- Have assistant turn on pacer generator with the above settings (remember it is non sterile)
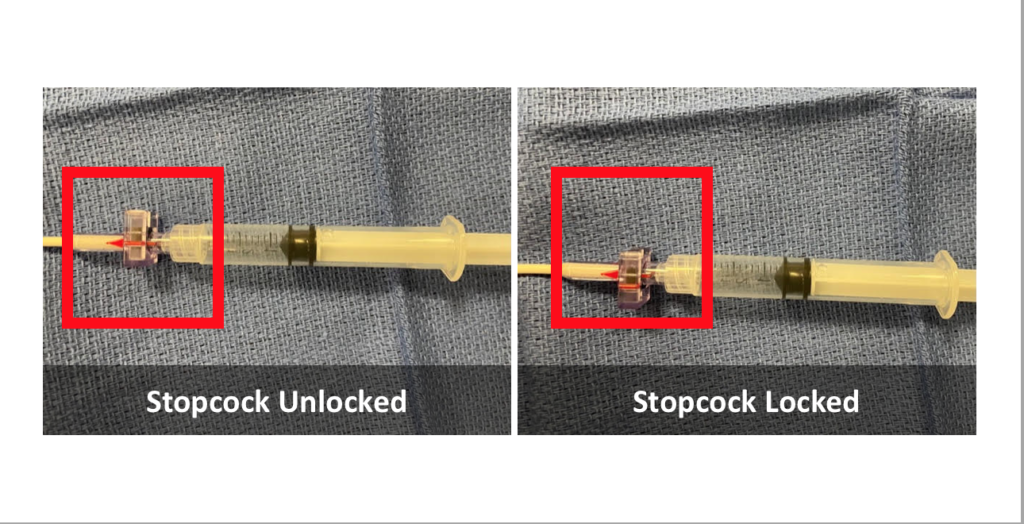
- Inflate balloon and lock purple stopcock (stopcock is on Swan, catheter see below image)
- Advance pacer wire to ~30-35cm (three black lines on pacer wire) while watching monitor for capture (STEMI pattern)
- Troubleshooting:
- if wire coils in RA, pull wire back, twist 180˚ towards patient’s right and re-advance
- if wire fails to capture, can adjust pacer generator settings, consider increasing output and decreasing sensitivity
- Verify capture by either palpating pulse or by pulse ox waveform
- Decrease output until there is no longer capture, then titrate up to the lowest effective output
- Deflate balloon and turn stopcock off
- Expand sterile sleeve
- Suture cordis and place sterile dressing
- Secure pacer wire to patient with tape (can dislodge easily)
Complications
- Misplacement—can verify with ultrasound or chest x-ray
- Ventricular perforation
- Dysrhythmias
- Pneumothorax
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)