We had a very ill patient recently. She was found down upstairs visiting her family member. She was calmly altered, not agitated but was in mild distress. Consciousness fluctuated. Tachycardic and hypertensive initially, then had more labile BP and some hypotension.
We had to intubate her due to poor MS and clinical condition. She coded in CT, we placed a central line on the CT table between her noncontrast head CT and her CT chest. We pushed an amp of Epi and ran out of the room for the CT chest. We were worried about dissection and PE in equal amounts. We could not get good cardiac windows on bedside Echo in room 9 prior to the CT.
She continued to intermittently lose her pulse and drop her BP. We confirmed bilat PEs on the CT when we saw NO contrast left her right ventricle. The CT tech noticed first and became worried the patient had no cardiac output (ie pulseless).
We rushed the patient back to room 9 and gave a tPA bolus (50mg) followed by infusion of 40mg. She was on pressors and heparin and improving. Dr Smith accepted her to Jewish for possible EKOS or even ECMO if needed. On arrival to Jewish a few hours later she coded and died.
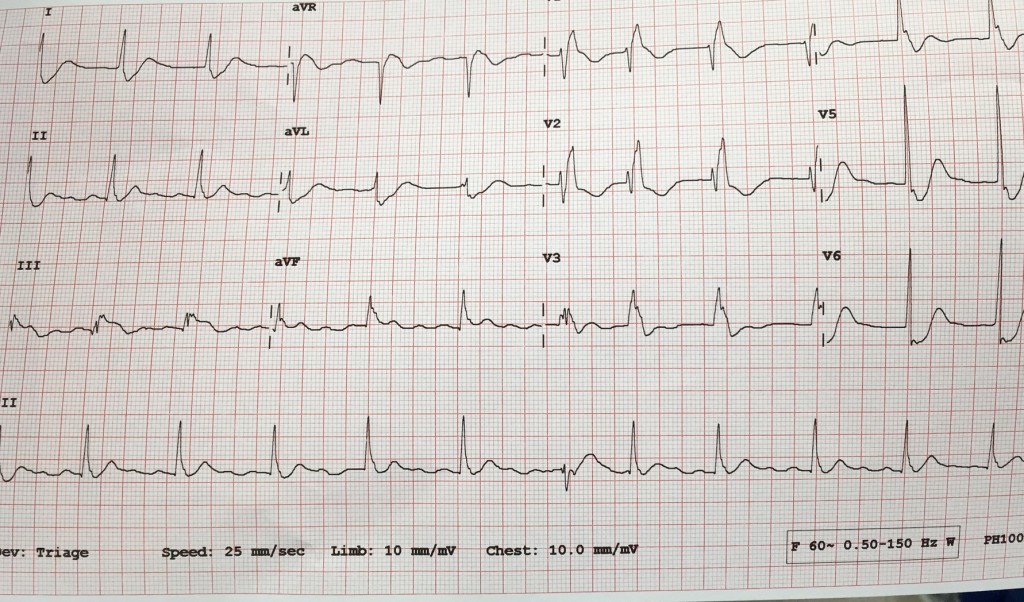
I was surprised when I found out she had died. Her O2 sat was improving, HR was decreasing, blood pressure was stable (though dependent on pressors). She received a large amount of crystalloid IV which according to some data might not have been optimal management. She also had the following ECG:
I think she was infarcting her myocardium. She likely had pulmonary infarction considering her poor oxygenation. She had coded a few times. She had a lot of strikes against her. Her BEST SHOT was going to a place with catheter assisted treatment for PE and ECMO if needed.
I am posting the case to let everyone know:
- How to manage sick PE patients (see post below)
- To use tPA in massive and in many cases of submassive PE
- TRANSFER sick PE patients to Jewish for EKOS/ECMO
- The decision to diagnose PE with RV strain on BEDSIDE Echo with no formal Radiologic testing will depend on your attending
This post from EmCrit / PulmCrit is a beautiful summary with potential dogmalysis related to PE management (see take home points below but do read the post).
In addition, here is a nice review article on catheter-based reperfusion treatment for PE with nice references for further reading.
Take home points from the Emcrit post:
- The only evidence-based intervention that seems to improve mortality in massive PE is thrombolysis. The primary goal of therapy should be administration of thrombolysis as soon as possible to patients without contraindication.
- Consider early stabilization of blood pressure using a norepinephrine infusion, administered peripherally if necessary.
- Volume administration may facilitate dilation of the right ventricle and hemodynamic deterioration.
- Intubation is very hazardous and should be avoided if possible. Patients die from cardiovascular collapse, and intubation may worsen this.
- For a coding PE patient consider 50mg alteplase bolus as well as an infusion of epinephrine. Patients can do well despite requiring CPR and high dose vasopressor infusions.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)