As we know, point-of-care ultrasound has become an extremely useful tool in the ED, allowing providers to glean disposition-altering information from a quick and non-invasive bedside study. On my ultrasound month, I helped out with a patient who presented with shortness of air for 2-3 days. The patient was a fairly poor historian, but she reported progressive dyspnea on exertion for several weeks along with cough and orthopnea. She had no formal diagnosis of COPD or CHF, but she had an extensive smoking history. I was asked to perform a bedside echo to help narrow down the differentials. The images I obtained demonstrated some classic findings of right heart strain, and I felt like this would be a good opportunity to review some of them.
- RV dilatation
As you can see in this parasternal long axis view from our patient, the RV is massively dilated in comparison to the LV. A normal RV : LV ratio is approximately 0.6:1. Anything larger than this is considered abnormal, with 0.6-0.9:1 representing mild enlargement, 1:1 moderate enlargement, and > 1:1 severe enlargement. When looking at the parasternal long axis view, you can use the “rule of thirds”. According to this, the left atrium, LV outflow tract, and RV outflow tract should be roughly the same size. In this video, the RVOT is clearly much larger than it should be. You can also get a sense of the relative sizes of the ventricles in the other three windows on transthoracic echo.
- RV systolic dysfunction
In our patient’s apical four chamber view, you can again appreciate the size of the RV compared to the LV. In addition, there appears to be relative hypokinesis of the free wall of the RV, suggesting there is systolic dysfunction. The right atrium enlargement seen in this video also suggests that this patient’s RV strain was more of a chronic process.
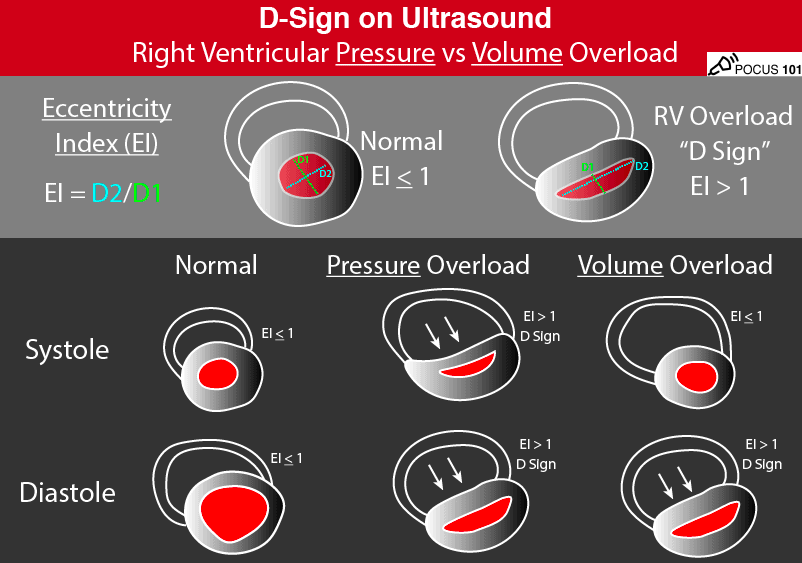
- Paradoxical septal wall motion
In a normal heart, the LV should be fairly circular in the parasternal short axis view, and the RV will appear more crescent-shaped. Additionally, the walls surrounding the LV should move inward equally during systole. In the setting of elevated RV pressures, you can often see the interventricular septum bowing in towards the LV, creating a “D” shaped left ventricle, as seen in the clip above. Interestingly, there are different variants of the so-called “D sign”, helping to distinguish between right ventricular pressure vs. volume overload. In pressure overload, the RV presses on the septum during systole AND diastole. Conversely, in volume overload, the septal bowing is much more pronounced in diastole compared to systole. Our patient has a D-shaped LV throughout the cardiac cycle, suggesting RV pressure overload.
- McConnell’s Sign
This finding refers to RV wall hypokinesis with apical sparing. As you can see in the video above, the apex of the RV appears to bounce up and down while the rest of the RV remains stationary. In the right clinical setting, McConnell’s sign is considered highly specific for acute pulmonary embolism. Disclaimer: this clip came from one of Dr. Nichols’s patients who was later found to have an extensive saddle embolus.
- Lack of respiratory variation in the inferior vena cava
The normal IVC diameter is less than 1.7 cm and there is a 50% decrease in the diameter during inspiration when the RA pressure is normal (0-5 mmHg). When the inspiratory collapse is less than 50%, the RA pressure is usually between 10-15 mmHg. If there is no collapse with respirations in a spontaneously breathing patient, this suggests markedly increased RA pressure > 15 mmHg. This is usually best evaluated using M mode, measuring the diameter of the IVC during inspiration and comparing to its diameter during expiration. Our patient has an enlarged IVC with almost no collapsibility throughout the respiratory cycle.
Conclusion
If you identify any of these findings on a patient in the emergency department, you should consider common causes of RV failure and strain, such as PE, pulmonary hypertension, left heart failure, ARDS, severe tricuspid regurgitation, volume overload, etc. Our patient received a CT PE in the ED, which was negative. She was subsequently admitted to the cardiology service, where right heart catheterization found evidence of severe pre-capillary pulmonary hypertension. After a few days of monitoring, she was subsequently discharged back into the world with a prescription for diuretics and follow up in the pulmonary clinic.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)