Pharmacy Lecture
Presenter: Nicholas Cottrell, Pharm.D
Intranasal Meds:
Adv:
- Ease of use
- Rapidly effective
- Relatively safe
Metabolism:
- Metabolized by liver
- Nasal meds bypass liver metabolism
- Optimizing drug intranasal:
- 0.2-0.3 ml, Never more than 1 mlà will cause post nasal drip
- Remove blood and mucous from the nose
- Use both nostrils
- Use atomized delivery system
Go to Treatment for Headache:
- Sphenopalatine Ganglion Nerve Block:
- Associated with trigeminal nerve
- Seen in migraine and cluster HA
- How to perform Sphenopalatine Ganglion Nerve Block
- 10 cm cotton tip applicator
- Anesthetic 1% lido
- 5 cc syringe with large bore needle to draw up anesthetic
Angioedema:
- Hereditary
- Recurrent attacks
- C1 esterase inhibitor deficiency
- Allergic reaction meds are ineffective
- Acquired Angioedema
- Rare
- Treatment:
- Green Zone: Minimal edema
- Observation
- Yellow: Moderate
- Watch, meds
- Red Zone: Immediate need for intubation
- Stridor
- Dyspnea
- Progressive deterioration
- Green Zone: Minimal edema
Intubations Hazards:
- Airway manipulation may worsen swelling
- Laryngeal edema will preclude use of LMA
TXA:
- TXA can work on bradykinin mediated angioedema
- 1 g IV push over 10 minutes, q4h PRN
- ADE: Thrombosis
- C1 esterase deficiency angioedema:
- 2 units of FFP initially, 2 units PRN
- Other meds:
- Icatibant and Ecallentide
- Take longer to work
- Not always available
- EXPENSIVE
- Icatibant and Ecallentide
Management of Obligate Neck Breathers
Presenter: Dr. Shawn Jones, Otolaryngology PGY-2
- Tracheostomy:
- Exteriorizes trachea to skin of neck for permanent gas exchange:
- Why:
- Severe OSA
- Head and neck cancers or masses
- Subglottic stenosis
- Ludwig’s angina
- Paralysis of vocal cords
- Prolonged ventilator support
- Benefits:
- Reducing need for sedation
- Improve patient comfort
- Reduce ventilator pneumonia
- Risks:
- Infections
- Bleeding
- Fistula
- Granulation tissue and scarring
- Tracheal occlusion:
- Mucus plugging
- Accidental decannulation
- Why:
- Exteriorizes trachea to skin of neck for permanent gas exchange:
Tracheostomy and Respiratory Distress:
1. Remove trach cap
2. Attempt to pass suction catheter to assess patency
3. Provide supplemental O2 (trach collar, BiPAP, bagging)
4. Replace uncuff trach tube with cuffed trach tube or cuffed ET Tube to provide PPV
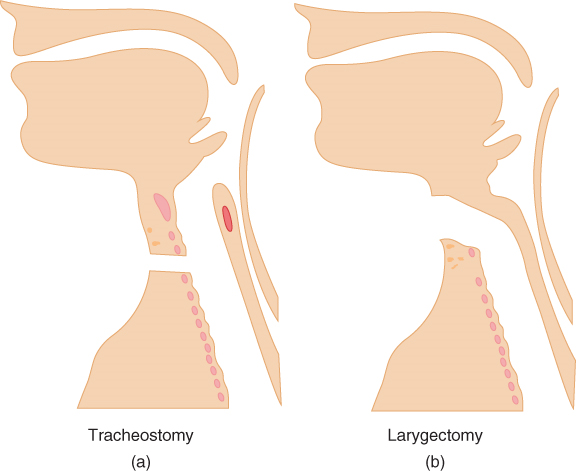
Image Source: https://aneskey.com/what-is-a-tracheostomy-what-is-a-laryngectomy/
Laryngectomy
- Larynx is surgically removed
- Upper airway no longer connects to trachea
- Trachea is fixed to skin to create permanent stoma
Indication:
- Cancer of head and neck
- Chronic aspiration
TEP = transesophageal prothesis – may be placed after laryngectomy to allow for speech
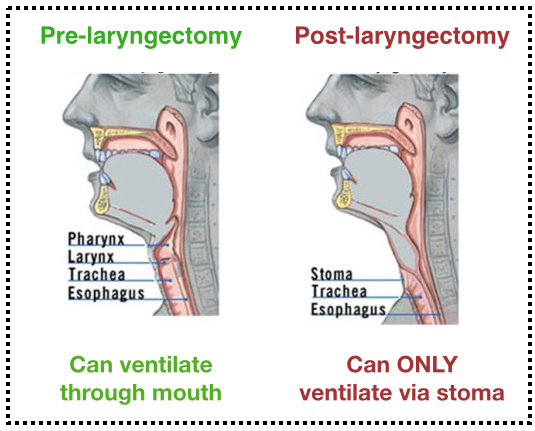
Image Source: https://sinaiem.org/dont-fear-the-tracheostomy/
Laryngectomy and respiratory distress:
- Provide supplemental O2: trach-collar, BiPAP, bagging
- Must place cuffed ET tube to provide PPV (lary tubes are uncuffed)
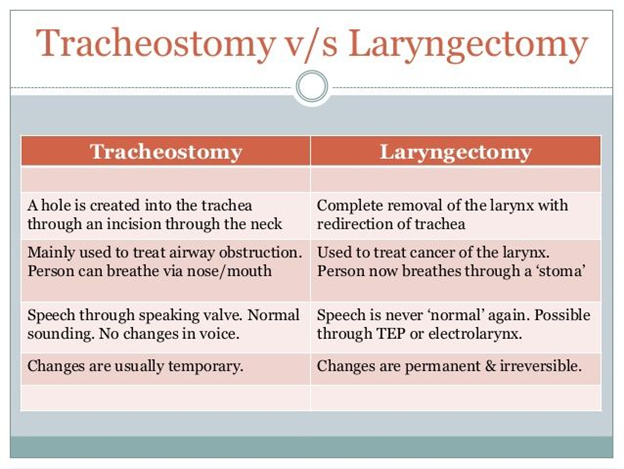
Image source: https://www.pinterest.com/pin/117586240255365772/
Pediatric Heme/Onc Emergencies
Dr. Julie Klensch, Pediatric EM Fellow
Hemorrhagic Disease of Newborn
- Vit K deficiency causes severe bleeding
- Onset usually during 1st week of life
- ICH, intrathoracic or intracranial bleeding, oozing from mucous membranes
Treatment:
- Vit K and FFP
- Transfuse for Hgb<7
- pRBC 10-15 ml/kg given over 2-4 hrs
- 10 ml/kg should increase Hgb by ~2
Hemolytic anemia
- Pallor, jaundice, dark urine, fatigue, dizziness
- Intrinsic vs extrinsic
- Evaluation: CBC, CMP, LDH, haptoglobin, direct/indirect bilirubin , Comb’s test in newborns
Sickle Cell disease
- Vascular occlusion
- Infection
- End organ damage
- Tx: analgesia and hydration
- Salmonella + sick cell patient = osteomyelitis
Dactylitis
- Vaso-occlusive crises of hands and feet; often initial presenting sign of SS disease
Splenic Sequestration
- Splenomegaly, thrombocytopenia, LUQ pain
Acute chest syndrome
- Infiltrate of CXR, chest pain, hypoxia
- Tx: ceftriaxone and azithromycin, IVFs, consider pRBC transfusion if respiratory support required
Stroke
- Management: CT, MRI, exchange transfusion
Avascular necrosis:
- Leg/hip pain, inability to bear weight
- Tx: analgesia and orthopedics consult
Infection
- Hyposplenia leaves patient at risk from encapsulated organism, specifically S. Pneumoniae
- Children < 5yo should be on prophylactic penicillin.
Thrombocytopenia
- Plt transfusion 5-10 ml/kg, rate dependent on urgency
- 1 U increase 5,000-10,000
Immune thrombocytopenia (ITP)
- Well appearing child, unexplained petechiae and bruising, isolated thrombocytopenia following viral infection
- Tx: IVIG, don’t transfuse plt
Neutropenia
- ANC<1500, severe ANC<500
- Fever + Neutropenia = septic work-up with administration of broad-spectrum antibiotics
Tumor Lysis Syndrome
- Initiation of chemotherapy; most common in leukemia or lymphoma (high cell turnover)
- Hyperkalemia, hyperphosphatemia, and elevated uric acid
- Tx: Allopurinol and hydration, Rasburicase for severe cases but expensive
Lateral Canthotomy – Procedure SIM
Presenter: Dr. Michael Carter and Dr. Ross Sizemore
Indication for lateral canthotomy: Ocular compartment Syndrome
- Most commonly due to blunt trauma
- Retrobulbar hematoma/hemorrhage
- Infection, orbital emphysema, FB (less common)
- Eye Pain, proptosis, difficulty open eyelids, pain/difficulty with EOM
- Perform pupillary exam, visual acuity, and tonometry (IOP>40)
- Order CT but do not delay treatment
- Irreversible vision loss may occur within 60-100 min if not treated
Globe rupture: contraindication to the procedure
Medical management:
- Elevate HOB, analgesia, and BP control, antiemetics
- IV acetazolamide
- Timolol eye drops
- IV mannitol
Pitfalls:
- Lack of early recognition and ophthalmology consultation
- Iatrogenic injury
- Incomplete resolution
Equipment:
- Chlorhexadine
- Lidocaine w/ epi
- Needle and syringe for lidocaine injection
- Straight mosquito hemostat
- Iris scissors
- Forceps
Procedure Tips:
- Angle sharps away from eye during procedure
- Recheck IOP after procedure
- Be aware of lacrimal gland if cutting superior tendon.
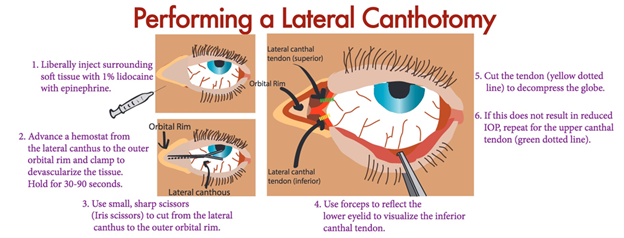
Image Source: https://www.tamingthesru.com/blog/annals-of-b-pod/ocular-emergency
Ceasing Resuscitation in the Pre-Hospital Setting
Presenter: Dr. Raymond Orthober
Termination of out of hospital cardiac arrest (OHCA)
- Non-traumatic patients
- 0.6% survival rate in those with ROSC >25 min CPR
- In most situations, ACLS initial resuscitation on scene is equivalent to ACLS offered in-hospital
- Goal: Gain ROSC and obtain good neurological outcome
Load-and-Go vs Stay-and-Play
- Trauma = Load-and-Go
- Medical = Stay-and-Play
Withholding resuscitation efforts: Evaluate life status
- Cold and stiff in warm environment
- Rigor Mortis
- Lividity
- Obvious mortal wounds
- Obvious signs of decomposition
- Valid DNR
Determination of death:
- Pupils fixed and dilated
- Apnea
- Pulseless
- Asystole in 2 leads
Exceptions to cease resuscitation in the field: cold water drowning, electrical injury, hypothermia
CPR underway & request to cease resuscitation:
- No bystander CPR
- No witnessed arrest
- No response after >6 min high quality CPR
- No shockable rhythm
- Asystole in 2 leads
- No ROSC at anytime
- 20-25 min CPR prior to request to cease resuscitation
EtCO2
- EtCO2 > 20 is a sign of life
- EtCO2 < 10 may be used to support termination of CPR
- Technical difficulties may lead to inaccurate EtCO2
- Use as complementary value in bigger picture of patient
Radio call – Questions to ask
- Valid DNR or MOST form?
- Witnessed arrest and/or bystander CPR?
- Definitive airway? iGel, LMA, ETT
- Any shocks delivered?
- ROSC at any point?
- Asystole at time of call?
- 20-25 min CPR?
- EtCO2<10
Termination of Resuscitation in Trauma
- Trauma = Load-and-Go
- All trauma patients should be transported except in rare circumstance of obvious mortal wound, no signs of life, and prolonged downtime
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)