I have recently seen many patients sent to the ED from urgent care centers and PCP offices for evaluation of hypertension. While true hypertensive emergency often leads to straight forward disposition, this condition is rare and much more commonly patients present with severe asymptomatic hypertension (sometimes referred to as hypertensive urgency). I will discuss an approach to management of these conditions below.
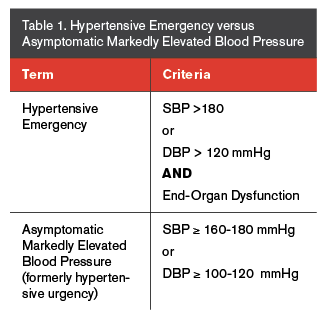
Image source: https://epmonthly.com/article/dont-let-hypertension-stress/
Common causes of hypertension:
- Medication noncompliance
- Pain
- High-salt diet
- Amphetamine or stimulant use
- Alcohol withdrawal or drug withdrawal
Less common causes of hypertension:
- Pheochromocytoma
- Thyroid Storm
- Intracranial hemorrhage
- Preeclampsia/Eclampsia
Special considerations in hypertension:
- Ischemic/hemorrhagic stroke
- Aortic Dissection
Hypertensive Emergency: Severe hypertension, commonly defined as BP > 180/120, with signs of end-organ damage.
End-organ damage:
- Neurological: intractable headache, vision changes, ischemic or hemorrhagic stroke, hypertensive encephalopathy or PRES
- Cardiac: chest pain, EKG changes or elevated cardiac biomarkers indicative of cardiac stress
- Pulmonary: dyspnea, pulmonary edema
- GI: abdominal pain, nausea/vomiting, transaminitis
- Renal: AKI, proteinuria, electrolyte abnormalities
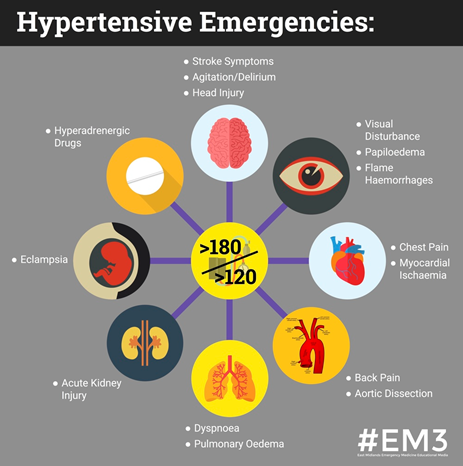
Image Source: https://em3.org.uk/foamed/8/6/2016/hypertensive-crisis
Work-up:
- CBC
- CMP
- EKG
- Troponin
- Chest X-ray
- Urinalysis
- β-hCG in females
- Consider Head CT if neurological symptoms
Management:
Treatment with IV anti-hypertensives and admission to appropriate service, usually medicine or cardiology.
Common IV anti-hypertensives:
- labetalol IV push (5-20 mg)
- hydralazine IV push (10-20 mg)
- nicardipine drip (start at 5 mg/hr and titrate to goal BP)
- nitroglycerin drip – specifically for acute pulmonary edema (see SCAPE management for dosing)
BP Goal: reduction in MAP by 10-20% in the first hour followed by gradual reduction in MAP by ~25% over the first 24 hours. Commonly a goal BP of ~160/100 achieves goal of 10-20% reduction.
*There is increased risk of cerebral and cardiac ischemia if lowering BP too rapidly
Exceptions:
- Hemorrhagic CVA and aortic dissection have specific guidelines for BP goals and rapid lowering
- Ischemic CVA allow for permissive hypertension
*Beta-blocker contraindicated in amphetamine intoxication and pheochromocytoma
- amphetamine intoxication – use benzodiazepine
- pheochromocytoma – use alpha-blockers (phentolamine)
Severe asymptomatic hypertension (hypertensive urgency): Severe hypertension, commonly defined as BP > 180/120, with no signs of end-organ damage.
*Some physicians strongly dislike the term “hypertensive urgency” and ACEP utilizes the term “asymptomatic severely elevated blood pressure”.
This is a diagnosis of exclusion. As an ED physician it is your job to first rule out hypertensive emergency.
Management of severe asymptomatic hypertension:
* The first 3 steps below should apply to any patient presenting for hypertension.
- Place patient in a quiet and relaxing environment (when possible)
- Administer patient’s home PO anti-hypertensives if not taken today
- Control patient’s pain and treat any underlying causes
- Consider additional PO or IV anti-hypertensives
- PO anti-hypertensives
- Captopril (6.25-50 mg)
- Enalapril (2.5-20 mg)
- Clonidine (0.1-0.2 mg) *Would avoid due to variable response
- IV anti-hypertensives
- labetalol IV push (5-20 mg)
- hydralazine IV push (10-20 mg)
- PO anti-hypertensives
- BP reassessment following administration
Goal BP prior to discharge:
- Ideally BP ~160/100
- In a completely asymptomatic patient, BP ~180/110 or even higher may be acceptable with appropriate follow-up
- No definitive recommendation exists for a blood pressure cut-off for which an asymptomatic patient must be acutely treated
- Many physicians have personal practice patterns and different comfort levels with this
Discharge Medications:
- If initiating home PO anti-hypertensives common medications include:
- Amlodipine (5-10 mg)
- Hydrochlorothiazide (HCTZ 12.5-25 mg)
- May considering increasing current home anti-hypertensive dose but would avoid this in most circumstances
- Once again, many physicians have personal practice patterns and different comfort levels with initiating or increasing doses of antihypertensives from the ED
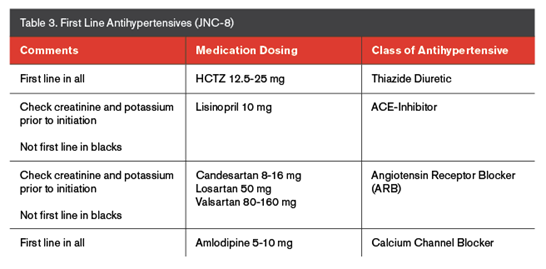
Image source: https://epmonthly.com/article/dont-let-hypertension-stress/
Follow-up:
- All patients should be provided resources for appropriate outpatient management
- Recommend repeat BP check within several days
- Recommend repeat renal function testing within 1 week if initiating anti-hypertensive therapy or increasing ACE or ARB
References:
- UpToDate: Evaluation and treatment of hypertensive emergencies in adults
- UpToDate: Management of severe asymptomatic hypertension (hypertensive urgencies) in adults
- TamingTheSRU: Clinical Practice Guidelines: Hypertension
- https://epmonthly.com/article/dont-let-hypertension-stress/
- https://em3.org.uk/foamed/8/6/2016/hypertensive-crisis
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)