US for Shoulder Dislocation and Reduction
- Approach
- Position the probe over posterior aspect of affected shoulder with indicator to patient’s left
- Measure distance between glenoid and humeral head
- Advantages: faster than XR, ~100% sensitivity
- Disadvantages: less sensitive for fractures, operator dependent, not full agreement on measurements
Fascia iliaca compartment block (FICB)
- This is different from the “femoral nerve block” and “3 in 1 block”
- FICB anesthetizes femoral nerve and lateral femoral cutaneous nerve
- Target: facial plane above the iliacus muscle. Infrainguinal.
- Inject 30-40 mL medial to femoral nerve using a 21 or 20 gauge spinal needle and extension tubing
- 0.2% or 0.5% Ropivacaine or Bupivacaine
- Analgesia onset within 30 min and lasts ~12 hrs
- If using 0.5% dilute 20 mL anesthesia with 20 mL NS
- ALWAYS calculate your dose
PE Clinical Pathway
- Categorization
- Massive: hypotension
- Submassive: RV dysfunction or myocardial necrosis w/o hypotension
- Non-massive or Sub-segmental: no hypotension, RV dysfunction, myocardial necrosis
- Utilize PERC and Wells criteria
- See full pathway posted separately
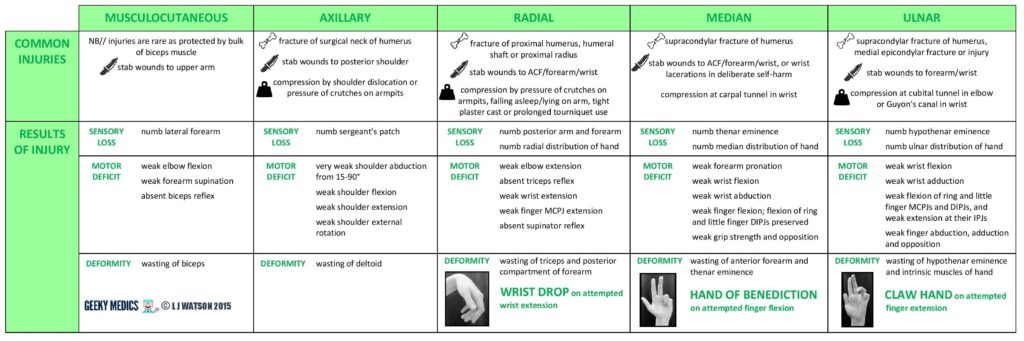
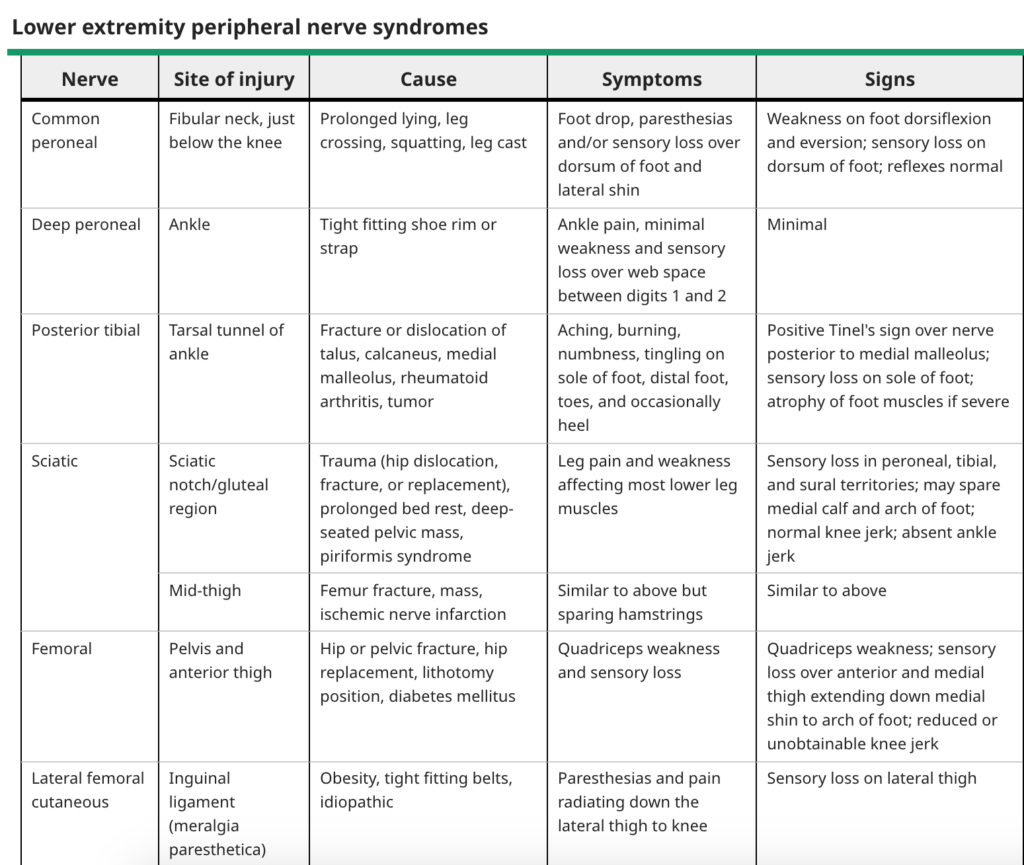
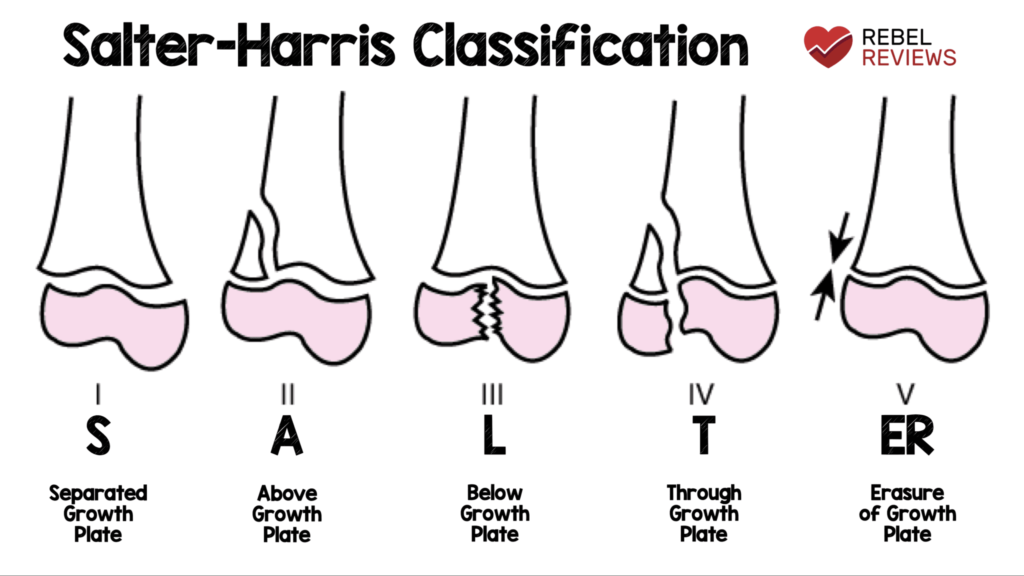
Extremity Trauma by Dr. Caleb Davis
- Clavicle fx – typically manage with sling
- May need OR if there is skin tenting or blanching
- Beware of scapulothoracic dissociation in AC joint injury. Requires OR
- Luxatio erecta (inferior dislocation) – to reduce, push the humeral head anteriorly under traction and then reduce like an anterior dislocation
- Scaphoid fracture – MRI is best imaging modality in the acute setting
- Pelvic ring injuries a thorough rectal and vaginal exam is indicated to rule out hollow viscus injury from the bone.
- Hip dislocation – need post-reduction pelvic CT to look for fracture fragments
- Femoral shaft fractures
- associated injuries common
- Need to make sure patient is adequately resusicated prior to operation to avoid 2nd hit injury to lungs. Get lactic and ABG to measure resus. Place on 2L NC.
- Don’t miss open fractures. Can be small “poke-hole”
- Knee dislocations – get ABG and CTA
- Tibial plateau fractures are often too swollen to fix initially.
- Fractures 2/2 GSW from 9mm rounds or lower are not considered open fractures
- Compartment syndromes
- pain out of proportion (first symptom)
- pain with passive stretch (most sensitive finding)
- Clinical diagnosis
Airway Assessment and Interventions
- Sedation/RSI
- Depth of sedation: mild, moderate, deep, general anesthesia
- Risk assessment with ASA class and LEMON
- SOAP-ME
- Suction
- Oxygen- preoxygenation and apneic oxygenation
- Airway equipment
- Positioning – put the towel roll under the occiput (NOT the shoulder) to align the tragus and sternal notch. Consider ramping the patient.
- Meds
- Equipment/EtCo2
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)