An interesting case from the Pediatric ED:
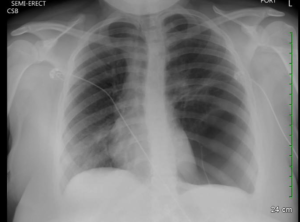
A mid teen female with a reported two year history of mild persistent asthma, presented with asthma exacerbation. She presented to an outside ED with two days of cough, wheezing and shortness of air which acutely worsened three hours prior to arrival. Upon initial presentation there, the patient was reported to be in moderate respiratory distress with increased work of breathing, tachypnea, and an O2 saturation in the 80%’s on room air. Lung auscultation revealed diminished breath sounds on the left with faint wheezing at left and right apices. She was placed on 3L nasal cannula with normalization of her O2 sats. She received an hour long course of albuterol and dose of Solu-Medrol, with moderate improvement in her symptoms. She subsequently received a chest X-ray which was concerning for a large left sided bleb/cyst with mediastinal shift to the right. Patient was subsequently transferred to us.
Further HPI and PMHx revealed that patient was diagnosed with allergic rhinitis in her early teens and diagnosed with asthma two years ago. She reported no history of ever being evaluated with a chest x-ray prior to current presentation. Over the course of the past two years she had been prescribed 3 courses of steroids and used albuterol approximately 2x per week PRN. Patient denied any other medical problems or smoking history.
A CT scan of the chest confirmed presence of large left sided pulmonary cyst.
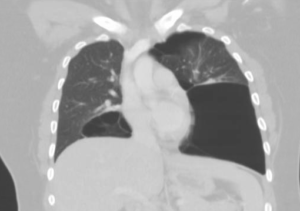
Patient was admitted and followed by both pediatric pulmonology and surgery. Inpatient workup included PFT’s and alpha-1-anti-trypsin (negative). She was eventually diagnosed with idiopathic giant bullous emphysema, otherwise known as vanishing lung syndrome. She later underwent bullectomy with improvement of her symptoms.
Bullous emphysema is often seen as a complication of COPD in adults, but rarely diagnosed in children with few case reports in the literature. Giant bullae can present asymptomatically, with progressive dyspnea, hypoxia or hemoptysis. Giant bullous emphysema is classified as occupying more than one third of a hemi-thorax, and is often initially mistaken as a pneumothorax on initial chest radiograph. As disease progresses, enlargement of the bullae fill with air and loss of lung function results as fibrous membranous surface of the bullae result in poor gas exchange. Bullae are at high risk for rupture and tension pneumothorax should be suspected if a patient develops worsening respiratory distress.
The learning point I took from this case is to step back and re-evaluate a patient’s presentation when things do not exactly add up, as in this case a teen with worsening asthma not responding to conventional treatment and little pcp workup in the past. This point is particularly exemplified in the pediatric population where we often see several low acuity cases each shift, often drifting into “auto pilot” mode, employing little critical thinking. Don’t forget, rare or more complex pathology may actually be responsible for the patients symptoms.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)