I had a fairly interesting patient back in November 2016 when I was at Jewish. I had picked up a patient with chief complaint of chest pain after an attending handed me the EKG below. The patient was being rolled back from triage to a room at the attending’s request. 42yo AAM with history of hypertension, hyperlipidemia, diabetes, sleep apnea and CAD status post CABG in 2008. The patient was complaining of chest pain that initially started when he was sitting at home watching TV about an hour prior to arrival. He described the pain as sub-sternal and radiating to his left arm. He had associated SOA, palpitations, and diaphoresis along with the pain. He was also nauseated since the onset of pain.
Pretty classic presentation here in a patient with previous heart disease. His initial EKG recorded in triage is below:
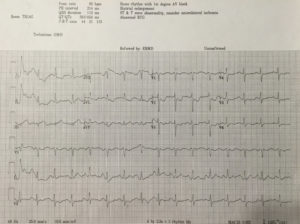
Upon review, you can appreciate that there may be ST elevation in III. Also, ST depressions are noted in the precordial leads along with ST changes elsewhere. My question to all of you based upon reviewing this EKG: Would you call this is a STEMI and would you activate the cath lab at this time?
The attending that I was working with at the time didn’t feel that we could definitively call this a STEMI based upon the first EKG. We examined the patient and collected his history after he was brought back. After labs were collected, the patient received nitro paste. Despite the paste, he continued to have pain. After approximately 15 minutes of being in the back, the patient reported that his pain was worsening. The decision at that time was made to get a repeat EKG. The repeat EKG is below:

So now what are your thoughts? There is obvious ST elevation in the inferior leads. There are also ST depressions in the precordial leads. This EKG was taken 34 minutes after the first EKG which was performed in triage. Through these two EKGs, you can appreciate the evolution of a STEMI. This patient was emergently taken to the cath lab at that time and underwent left heart cath. He underwent an impella-assisted PCI to his SVG-PDA and was started on dual anti-platelet inhibitors. Following his PCI, he also had an episode of wide-complex rhythm which resolved after receiving amiodarone.
So this patient who was found to have a STEMI on his repeat EKG had presented with an initial EKG that was non-diagnostic for his condition. Did this affect his outcome in any measure? What can we learn from this?
According to a 2013 study conducted by Riley et. al, in a national sample of patients diagnosed as having STEMI (41,560 patients), 11.0% had an initial non-diagnostic ECG. Of those patients, 72.4% had a follow-up diagnostic ECG within 90 minutes of their initial ECG. There did not appear to be clinically meaningful differences in guidelines-based treatment or major inhospital outcomes between patients diagnosed as having STEMI on an initial ECG and those diagnosed on a follow-up ECG.
So, did the additional 30 minute delay in activating the cath lab affect this patient? Likely not. However, what this case reinforces is the importance of a repeat EKG as 11% of these patients likely will not have STEMI on their first EKG.
References:
Am Heart J. 2013 Jan;165(1):50-6. doi: 10.1016/j.ahj.2012.10.027. Epub 2012 Nov 21. Diagnostic time course, treatment, and in-hospital outcomes for patients with ST-segment elevation myocardial infarction presenting with nondiagnostic initial electrocardiogram: a report from the American Heart Association Mission: Lifeline program. Riley RF1, Newby LK, Don CW, Roe MT, Holmes DN, Gandhi SK, Kutcher MA, Herrington DM.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)