Late 20s female w CC of chest discomfort and palpitations, n/v x 1 days. No recent illness, no fever/chills/diarrhea. Says the episodes come on abruptly and last less than a minute. No h/o early cardiac disease or early death in family. Says she feels short of breath with the episodes and her chest feels tight. Denies tunnel vision. Denies syncope but feels like she could pass out. ROS o/w positive for anxiety (grad student). Denies T/ETOH/D. Social history o/w irrelevant. No allergies. Only medicine is OCP. Exam is unremarkable (heart normal, lungs clear, appears well).
What would you order on this young patient with this complaint? How would you document it?
I have recently seen a few charts in this and similar patient presentations that gave me pause. I’ve seen workups from EKG alone to the full cardiac rule-out and everything in between. The only true unifying theme, and I think rightly, the most important test is the EKG (aside from a pregnancy test).
And most of the charts have a documented EKG. Ok. No problem there. Below is an example of a chart documented on a <30yoF patient with Palpitations…
“NSR, Rate 85, Normal P waves. No S/T wave changes. Normal QTc. No ischemia. No EKG for comparison. “
The problem with this? Aside from a few parts, it is mostly irrelevant to the life or limb threatening abnormalities that we are looking for in the EKG. Sure, it will bill just fine, but I worry that there a few among us who aren’t SPECIFICALLY looking at the EKG in the palpitations patient for common causes of palpitations. I mean, really, how many of us see MIs present as palpitations?
So what should you look for in an EKG in a palpitations patient?
- Rate (tachy or brady or no?)
- Blocks
- HOCM
- Brugada
- AVRD
- Prolonged QT (cong. QT) or Short QT (why?—AVRD)
- WPW
- Ischemia
Now lets talk about the EKG abnormalities found in each:
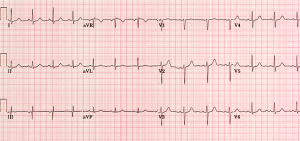
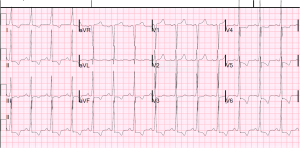
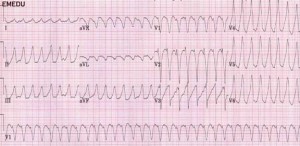
HOCM—About 90% of HOCM pts have an abnormal EKG. Remember, these are often young folks, so their ekg should be pristine. The etiology is a hypertrophic septum, so characteristic LVH is seen (V4R wave is “off the chart”), as well as deep, narrow q waves laterally. Occasionally flipped, broad T-waves are seen. There is also an apical variant that shows GIANT TWI in septal and lateral leads… you’ll know it if you see it, it looks grossly abnormal. But HOCM itself can be much more subtle. Look for Q waves and LVH then listen to their heart and refer to cardiology for an echo. Both of the below are pretty obvious, the second one is the GIANT TWI i was talking about. Not a lot of things do that.
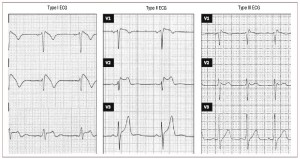
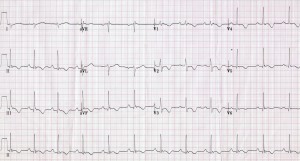
Brugada— 50% familial, most present >20yo but can be seen at birth. In brugada, you’re looking at leads V1-3, looking for a Right bundle branch block and either “coved” (st elevations with long, flat ST-segment that looks like a ski-slalom) or the “saddle type” (which is way less common and looks a lot like, well, a saddle. But remember there is STE there too which makes a side of the saddle, then the T-wave makes the other side of the saddle. This sometimes looks like a STEMI, except in a patient without chest pain and then you notice the saddle shaped concave ST segment and the CC and family history and you can smile because you didn’t activate the cath lab. Also, these patients can have EKGs that show brugada pattern SOMETIMES and not other times. Look for the ski-slope and the saddle. Hop aboard this saddle and you’re going to need a defibrillator, as anti-arrythmics don’t change mortality much….
This image says there are 3 types. OK, well, that’s true and all but seriously, it’s still a saddle, so you shouldn’t be led astray.
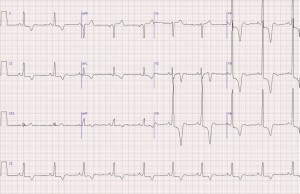
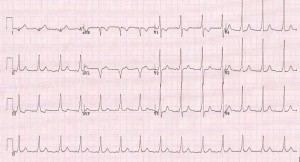
AVRD- What the what? AVRD stands for arrythmogenic right ventricular dysplasia, and basically their RV gets filled up with fat and cartilage during development. This is not so good. These folks may have exertional chest pain (it’s a cardiomyopathy). And, because it’s a structural heart disease, most of them will have EKG abnormalities (~90%). The most specific finding is an EPSILON wave, which is a little puny looking bump after the QRS that looks like a little P wave but is out of place and behind EVERY QRS. These are hard to catch, so you HAVE TO LOOK FOR IT IN PARTICULAR! Also, remember, not every Osborne wave is AVRD (is the patient hypothermic?) Occasionally this will make the QT interval short, but it isn’t reliable. Other, less specific findings are TWI in V1-3 that looks like a juvenile pattern… but remember juvenile pattern should go away when the patient becomes less juvenile. So if they have TWI in percordial leads an they are >20 and have palpitations or syncope… PANIC. No, but really, they probably have AVRD. And the syncope was probably VTACH. But they’re good now, right? Give them a defibrillator too.
Oh, crap. That’s what happens when you send the patient home without looking for AVRD.
Congenital Prolonged QT-– Ok, so a bit of an update to our usual shortcut “half the R-R rule,” in Academic Emergency Medicine in October 2015, some folks published a retrospective review of some cases of EKGs with prolonged QT and non prolonged QT, and found that our quick half the RR interval thing is about 88% sensitive (r/o prolongation) but only 53% specific. Which ain’t terrible, but its also not super good (12% aren’t ruled out). Of course, what the study failed to highlight but is written and useful is that the ½ RR rule is 100% sensitive (in this study) if the HR was >60. So my take is, if they are brady, calculate it yourself, and if not, 1/2RR is good to go. Which is what I think most of us do anyway. Three cheers for studies confirming our guesses!

WPW—Not much to say here. You know this. And you damn well should be documenting it. That PR interval is short because your patient is dying for you to find his delta wave.
ACS– Well, this is what we do.
Blocks- P before every QRS, QRS after every P. Intervals.
So… how should you be documenting these EKGs? With the same attention to the life and limb threatening abnormalities you are looking for on your history (early family death) and exam (murmur?). I can’t say what is right or not, but below is how I would document that EKG on our patient from earlier (NSR, rate 85, No STE/D, No TWI, no definite EKG evidence of WPW/AVRD/CongQT/blocks/HOCM).
Cheers.
Images:
https://meds.queensu.ca/central/assets/modules/ECG/Normal_ECG.bmp
http://hqmeded-ecg.blogspot.com/2014/06/history-of-hypertrophic-cardiomyopathy.html
http://www.doctorshangout.com/photo/hypertrophic-cardiomyopathy-apical-variant-yamaguchi-s-syndrome
http://hqmeded-ecg.blogspot.com/2013/05/brugada-pattern-induced-by-tricyclic.html
http://www.revespcardiol.org/imatges/255/255v62n11/grande/255v62n11-13145482fig1.jpg
http://www.geneticheartdisease.org/jpegs/avrd_figureone.jpg
http://www.heartpearls.com/wp-content/uploads/2009/07/ARVC.jpg
http://www.crkirk.com/thumbnail/arrhythmias/images/svt/ECG_WPW.htm
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)