The patient is a 20s y/o AAF, multip, last normal period 3 weeks ago (definite date), who presented to another facility with spotting and occasional moderate bleeding for about a week with 4 days of crampy pelvic pain, worse on the left than the right. There, she was diagnosed with trichomonas and treated empirically for gonorrhea and chlamydia. She had a positive pregnancy test and reportedly had transabdominal and transvaginal ultrasounds. She stated they told her she definitely had a pregnancy in her left tube. She was given instructions to see her regular doctor in 48 hours for a repeat evaluation and discharged.
It is at this point that the big red flashing lights in my head go off and I think to myself “Wait, WHAT? Someone DISCHARGED a confirmed ectopic? No way. Maybe they said it was a possibility and she misinterpreted.” Whatever the sequence of events, all that mattered was that I get the records and do an ultrasound myself.
Her records came in from the other ED after a couple of attempts (as per usual). A few things that I learned from her records:
1. she was indeed told that she had an ectopic and that she should see her regular doctor or OB in 48 hours.
2. she did get treated for STDs.
3. sure, she had an ultrasound, but there wasn’t any interpretation available unless I called and had them hold the phone up to the speaker (didn’t have time to do this).
4. my dislike for paper charts is warranted when I can’t read what someone says about my patient.
Initial vitals normal with a HR 100, BP 118/78
She was tender in the LLQ and suprapubic areas without peritoneal signs. Cervix was closed, she had a small to moderate amount of dark blood in the vaginal vault, and had uterine and left adnexal tenderness on bimanual exam.
I started fluids, gave her some meds for her nausea, and put in all the usual orders.
Labs:
-WBC 13.8 (88% Neut)
-Hb 9.6
-CMP unremarkable
-U/A positive for blood/protein/ketones but micro negative
-Quant 12000+
-Swabs + for trich
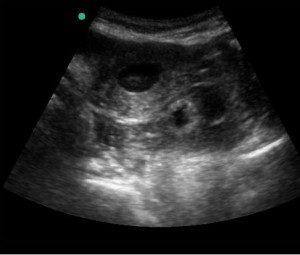
And then came the ultrasound:
A few things about this caused even more red light flashing: first, how could a gestational sac be THAT SIZE in someone whose last period was 3 weeks ago? Second, what was that OTHER thing behind the uterus on the left? Third, if the sac was really that big, why was there no pole?
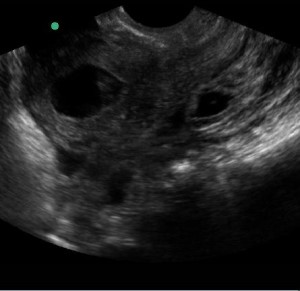
The transvaginal exam was more or less to confirm my suspicions that this was not normal. I knew that my plan was now to call the specialists with the fancy machine and adnexal expertise. I couldn’t actually get a GOOD view in two planes (sorry, Dr. O’Brien!) due to patient discomfort, but this one was good enough.
I hadn’t seen any free fluid in her pelvis on either exam. However, when OB came down, they found some. They confirmed my suspicions and admitted the patient to go to the OR.
In my brief lit search just prior to posting, I found that this pseudosac finding is not extremely common (the average reported frequency is about 10% of cases). I feel like this patient’s story would have raised enough red flags to make me uncomfortable sending her home without OB involvement even without the ultrasound, but the date/quant discrepancy coupled with a sac that was definitely not consistent (even though it WAS in the uterus) clinched the diagnosis for me.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)