So this is a case I thought was interesting that I had in the department back in May. We all know that the most common EKG finding in the setting of PE is sinus tach, however the pimp question that is also asked is the finding of S1Q3T3. While I can easily recite the alphabetic-numeric code S1Q3T3 by heart at the drop of a hat, I had never seen one and honestly thought I never would. I thought finding S1Q3T3 was likely as rare as surviving a ED thoracotomy (OK maybe not that rare). So on to the case.
39 year old female presents to the ED complaining of SOA and cough for the past two weeks. Cough was productive of green sputum, no fevers, and she does complain of some chest pain which sounds pleuritic in nature. Initial vitals HR 118 BP 111/73 RR 16 O2 97% room air. As I get into her PMH she says she has a history of multiple PEs with an IVC filter placed 1 yr ago because apparently she wasn’t very good at remembering to take her coumadin. She has had a hypercoagulability workup which was negative, no recent travel, no estrogen use.
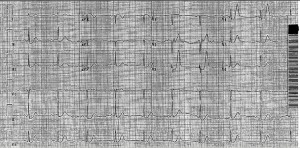
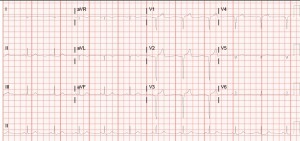
So at this point with a history of multiple PEs, tachycardia, SOA, and pleuritic chest pain I am thinking I am going to scan this lady. Even though she had a IVC placed a year ago, she is still saying all the right things for PE. So while the CTPE protocol was cooking I got an EKG and there it was, S1Q3T3!
Needless to say I was pretty excited and immediately showed the rotating intern next to me who clearly didn’t share my enthusiasm. When I compared this new EKG to a past EKG a month ago she did not have the S1Q3T3.During her admission a month ago, when she had a normal EKG, she had a CTPE showing a chronic PE. This time when her CTPE came back the read was Acute on Chronic Pulmonary Embolism. So a month ago she had a chronic PE with a normal EKG and at this visit she had an EKG with S1Q3T3 and a acute on chronic PE. Out of curiosity I dug through her medical history a little bit more and found that this patient had multiple prior admissions for PE with multiple CTPE protocols and EKGs. What I found was that whenever this patient had a CT read of Chronic PE she had a normal sinus rhythm EKG. However, whenever she had a read of Acute on Chronic PE (which was 4 times!) she had a EKG showing S1Q3T3, dating all the way back to 2012. Yea, apparently this lady has been hanging out with a chronic PE in her distal right main pulmonary artery since 2012 and every once in a while she will throw a new small PE, even with an IVC filter.
So after doing a little bit of thinking and a little bit of reading it made sense. The EKG finding of S1Q3T3 is indicative of right heart strain, in this case resulting from an acute PE. So this patient’s heart has adapted to her chronic PE, however every time she throws a new PE she has an element of right heart strain which can be seen on her EKG as S1Q3T3.
I just thought this was pretty interesting to actually see the physiologic and mechanical adaption and strain this patient’s heart was undergoing being clearly demonstrated on her EKG. Also I learned that S1Q3T3 is not like a q wave after an MI in that it stays on the patient’s EKG, it is a finding that comes and goes depending on the patient’s presentation.
Anyways I thought this was a pretty cool little case and figured I would share. Hope you all enjoyed.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)