Great case I had in December. Overall good month, but this case was especially interesting, and humbling. It combines the excitement of chest pain, the enigma that is leg weakness, and humbling realization of a life threatening diagnosis.
Working in the ED one day and the psychiatry intern goes to see a patient. Routine patient, who had presented with right leg tingling and weakness that made it all the way to the back of the ED. Bed 15. Basic labs pre-ordered as well as a chest X-ray for a brief episode of chest pain that the patient told triage. Of course, the sixth vital sign, an ekg. Intern is with the patient for about 5 minutes and returns. He tells me that he is concerned that the patient is sick and wants me to see the patient sooner than later. He is concerned for possible stroke due to right leg weakness and pain. I tell him of course and I go see the patient.
HPI: 58 y/o AAM with hx of seizures on Dilantin but no other medications or PMH presents with chief complaint of right lower leg pain and tingling. Patient states that while at work today, he was lifting boxes and felt a sharp chest pain that started in the middle of his chest and radiated to between his shoulder blades. It then shot to his pelvis and went away. He went back to work for about 10 minutes then started to have right leg pain. He tried to drive to the hospital, but had to stop and call an ambulance due to sever RLE pain. All other symptoms had resolved at this point. No n/v, diaphoresis, dizziness, loss of bowel or bladder.
Pertinent Hx: NKDA, 30yr pack hx of smoking, dilantin.
Vitals: BP: 148/62, HR 66, RR 18, O2 100% T 98.5
Significant Physical Exam –
RRR, no m/r/g, CTAB, abd soft, nt, nd, no bruit, no pulsating mass
RLE strength 4/5, LLE 5/5.
No DP, PT, popliteal, or femoral pulse in the right leg.
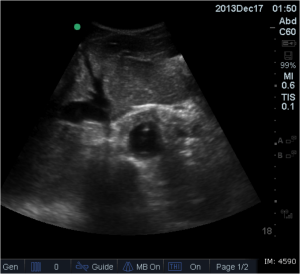
At this point I was concerned. I excused myself and got the bedside ultrasound. In my head I wondered was this just a arterial occlusion, or was this something greater?
Well this is when I started to sweat. I tell the patient what I think my diagnosis is, and head back to my desk to get orders going. At this time I review the labs and chest X-ray.
CBC – WNL, CMP – K 3.3, UA WNL, Troponin Neg, Tox Screen Neg, Coags neg.
Chest Xray –
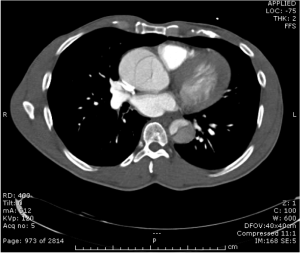
Any more concern? At this point I ordered a CTA of the Chest/Abdomen/Pelvis as well as called the surgery team. I wanted to get them involved early in the case that the patient deteriorates. I assessed the patients blood pressure at at the time was 130/60 and HR 58. I got the nurse to get the patient to the CT scanner as well as discussed with the trauma team. At this time patient had stable vital signs and pain controlled with morphine. Trauma evaluated and the CT resulted.
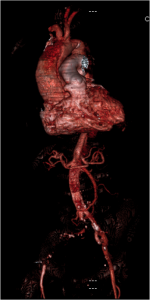
We now have our diagnosis. When patient got back from CT scanner, his blood pressure was increasing and now 150/80 and HR 68 with increasing pain.
Esmolol gtt was started, arterial line place, and the patient was transferred to another local hospital to undergo cardio-thoracic surgery for repair.
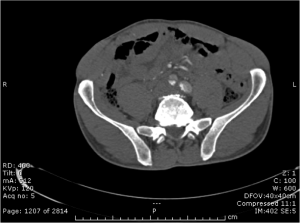
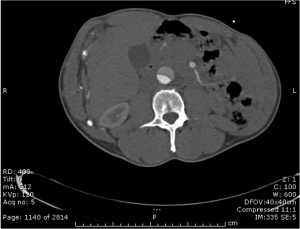
Diagnosis – Aortic Dissection from the level of the aortic valve down through the bifurcation of the iliac arteries. From the one slice, you can see he had no flow to the right leg. CTA demonstrated some collateral from the gastrics, but overall no flow.
Patient outcome – survived surgery. Otherwise have not been able to follow-up past that time. I shared this case because I feel it is a good representation of a case where easy bedside diagnostics can give you the diagnosis early and lead to your diagnosis. With the chest X-ray as well as the bedside ultrasound, we knew what the patient had. The CTA was just icing on the cake. Never be afraid to use the ultrasound. If it had been negative, this could have gone a completely different direction. Credit to the psychiatry resident for getting me involved early.
Use the ultrasound. Use it early. Diagnose early.
![Room9er ["Room Niner"]:](https://room9er.com/wp-content/uploads/2020/03/cropped-Screen-Shot-2020-03-08-at-3.16.16-PM.png)